The purpose of this blog is to debunk the 5 most common myths about MRIs and x-rays!
Looking for rehab or performance programs? Check out our store here!
Myth #1: Imaging Shows The Cause of Pain
Here’s a common scenario – You begin experiencing pain, so you receive imaging, such as an MRI, that discovers an abnormality. Therefore, this imaging finding is showing what’s causing your pain.
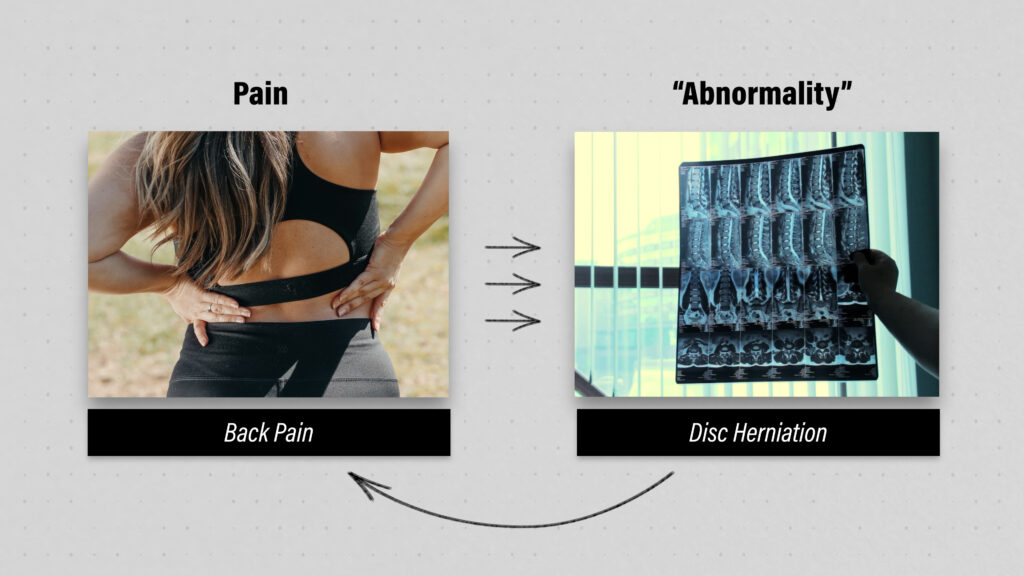
But what if I told you that these so-called “abnormalities” are actually quite common in people without symptoms?
For example, a study by Horga et al in 2020 had 115 uninjured adults with a median age of 44 undergo imaging of their knees and concluded that “nearly all knees of asymptomatic adults showed abnormalities in at least one knee structure on MRI,” including 30% presenting with meniscal tears.
A different study by Barreto et al in 2019 evaluated 123 individuals who had one-sided shoulder pain and concluded that “most abnormal MRI findings were not different in frequency between symptomatic and asymptomatic shoulders.”
Since there are countless examples of different diagnoses at different body regions, researchers and healthcare professionals are now referring to many of these findings as normal, age-related changes (similar to wrinkling of your skin or graying of your hair).
Imagine getting in a car accident, developing low back pain, and then receiving imaging that finds an abnormality.
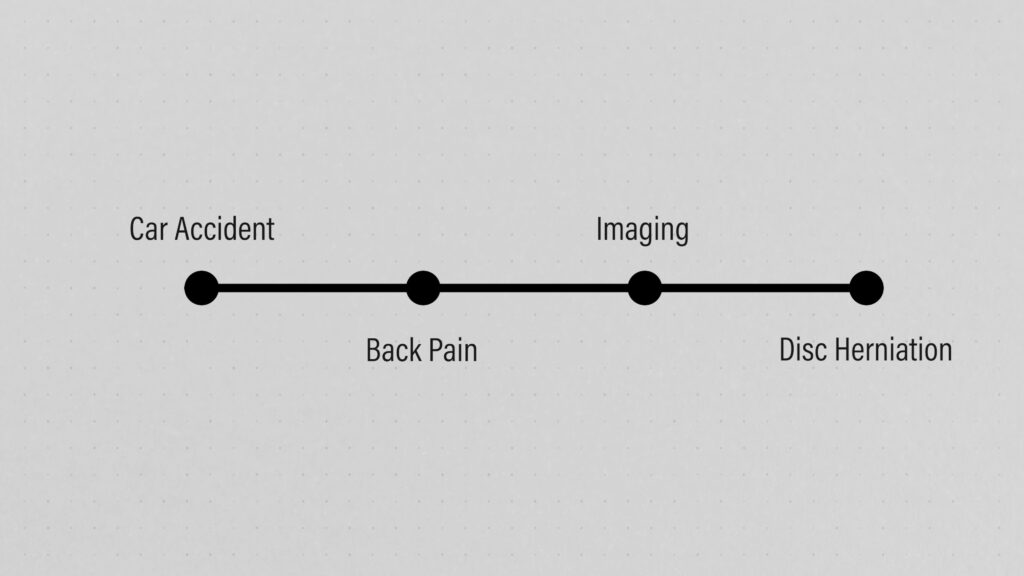
Based on the information I just presented though, you should understand that the imaging finding may have been present prior to the accident and is likely unrelated to the current episode of symptoms.
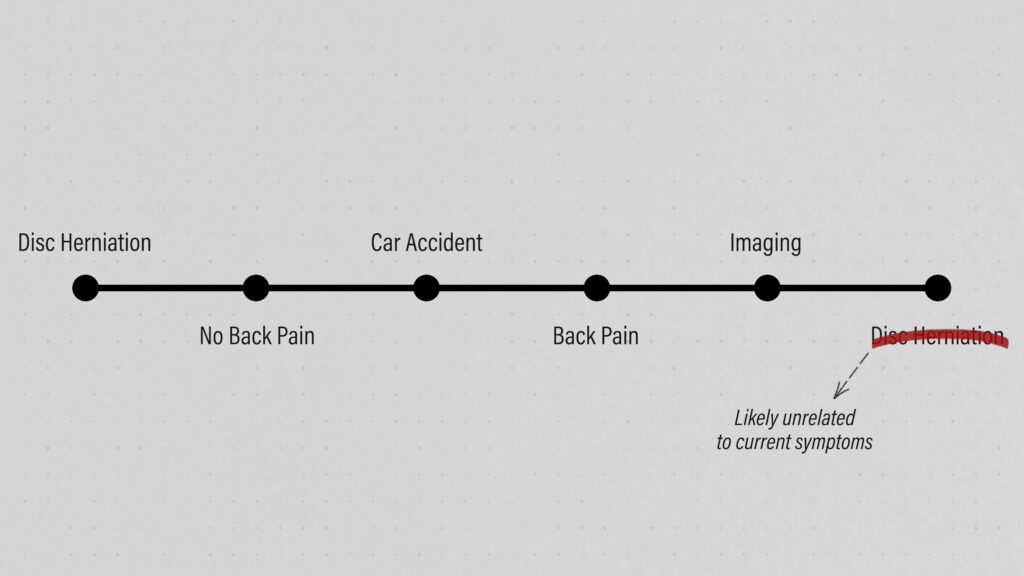
This doesn’t mean that your pain isn’t real, we just can’t always see it with a picture.
Generally when it comes to imaging, if you’re looking for a connection, you’re going to find it.
Myth #2: Imaging Predicts Your Outcomes
What if your symptoms are correlated with your x-ray or MRI? Does that mean that the worse the imaging looks, the worse your symptoms, function, and long-term recovery will be?
Not necessarily.
For instance, bigger disc herniations or greater nerve compression doesn’t automatically mean you’re not going to recover as well. You might have a large disc herniation, but get better quicker than someone with a smaller disc herniation.
Similarly, symptoms associated with osteoarthritis don’t always match the degree of change on imaging. You can have minimal-to-no pain or loss of function, yet have significant bone spurs and joint space narrowing.
This is one of the reasons I think medical professionals shouldn’t be telling patients that their knee is “bone-on-bone” or their hip x-ray is the “worst I’ve ever seen.” Oftentimes, the impression that those words leave are far more harmful than whatever the imaging actually shows.
Myth #3: If You Fix The Image, You Fix The Pain
Despite what I’ve already discussed, it stands to reason that if you’re experiencing symptoms and you have imaging findings that correlate with those symptoms, then fixing those imaging findings will fix your symptoms.
Unfortunately, it’s not always that simple.
For example, a systematic review by O’Connor et al in 2022 concluded that arthroscopic surgery for degenerative meniscal tears “provides little or no clinically important benefit in pain or function, probably does not provide clinically important benefits in knee-specific quality of life, and may not improve treatment success compared with a placebo procedure.”
A paper by Persson et al in 1997 compared surgery, physical therapy, or a cervical collar for the treatment of cervical radiculopathy (which is neck related nerve pain, muscle weakness, and sensory changes) and concluded that “the 1-year outcome shows no significant differences between surgical and conservative therapy.”
I want to point out that I’m purposely only providing a couple of examples per section to keep the blog shorter, but as I mentioned earlier, there are numerous studies to show similar findings for a variety of diagnoses at different body regions.
Since imaging doesn’t always show the cause of pain or determine how well you’re going to do in the long run, this information hopefully makes sense and highlights two things:
- The importance of trying to match your clinical presentation with your imaging findings to determine your true appropriateness for surgery or other treatments. I say “trying” because I’ve already pointed out that it’s not always possible.
- Like a cut on your skin, many conditions can heal or get better completely on their own. And like a cut on your skin, you might end up having a visible scar, but that scar usually doesn’t cause lingering issues and may even fade away over time.
Myth #4: Imaging Dictates Rehab
How do you treat someone with a disc herniation? If you’re a physical therapist or someone who has searched for the answer to this question in the past, your initial thought might be to perform repeated extensions, or repetitive arching of the low back. And you might be right.
But I didn’t tell you if the disc herniation was in the low back or the neck. I also didn’t tell you if the person even had symptoms. If they did have symptoms, what if they felt better with repetitive flexion, or bending forward?
We need context!
Two people can have the exact same diagnosis based on their imaging, but that snapshot of their anatomy doesn’t inform us of their age, lifestyles, goals, sleep habits, what makes their symptoms better, what makes their symptoms worse, etc.
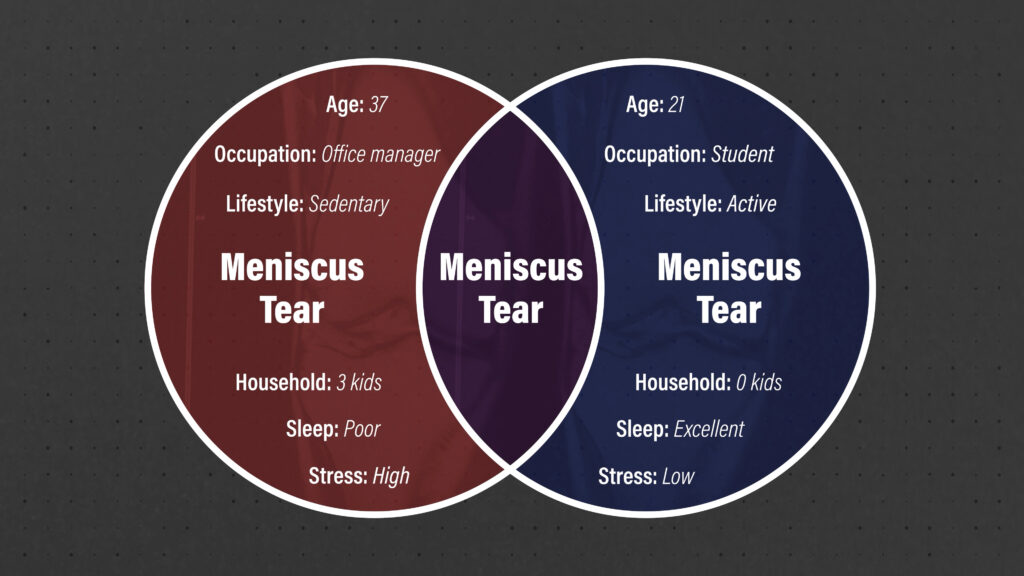
If you just fixate on an image, and the supposed implications of that image, you might create a self-fulfilling prophecy.
- “My knee is bone-on-bone, so I can’t run.”
- “There’s a herniated disc at L5-S1, so I stopped going to the gym.”
- “I have a pinched nerve in my neck, so I don’t play golf anymore.”
But I want you to remember 4 things:
- Most so-called “abnormalities” are common in people without symptoms.
- Imaging doesn’t necessarily predict long-term outcomes.
- Some imaging changes can resolve on their own.
- Even when imaging changes don’t resolve, symptoms and function can improve.
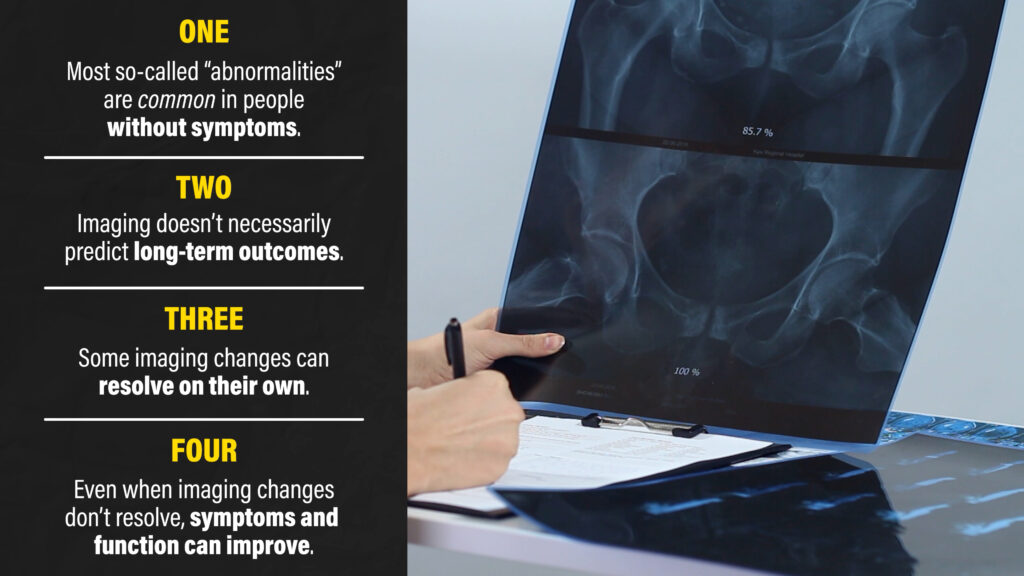
Imaging influences rehab the same way a compass influences navigation – as long as it’s not faulty, it may point us in the general direction we’re trying to go, but it won’t tell us the best path to get there or how to negotiate all of the obstacles along the way.
Don’t let a picture be the thing that holds you back in your rehab journey.
Myth #5: Imaging Never Matters
Imaging does matter when applied and explained appropriately.
Following trauma to the ankle and foot, an evidence-based guideline, known as the Ottawa Ankle Rules, determines if you need x-rays to rule out the possibility of a fracture. There’s a similar set of rules for the neck. These validated procedures help medical doctors avoid the use of excessive imaging in these scenarios, while capturing the people who need specific medical management for their injuries.
Most low back pain is unrelated to serious pathology, but there are the rare cases when it’s related to cancer, an infection, or something else that requires immediate medical attention. X-rays and MRIs are extremely important in these situations.
And there’s times when imaging influences rehab or is used as part of the decision-making process for determining the appropriateness for surgery.
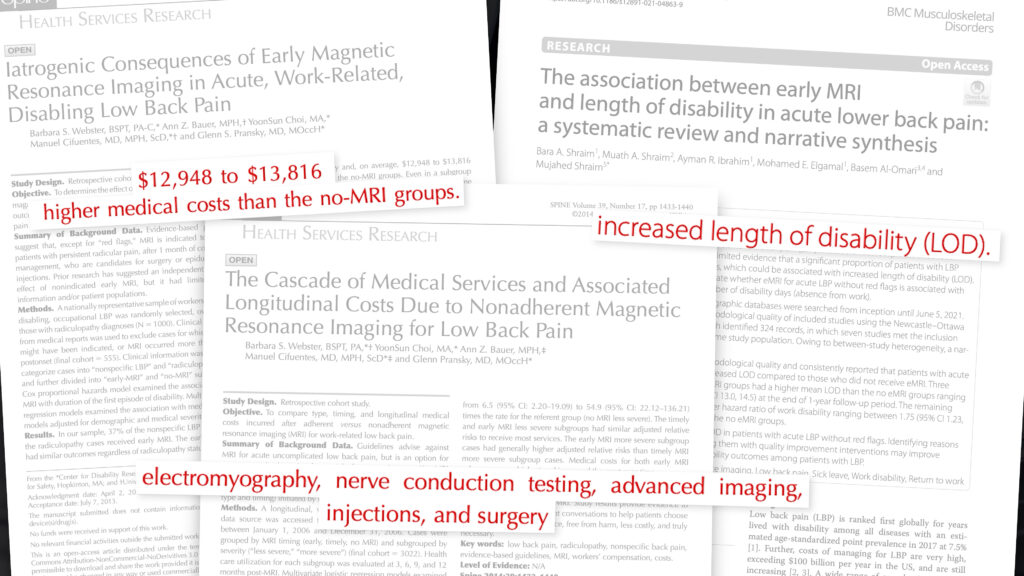
However, the purpose of this blog is to debunk common myths because the overutilization of imaging can actually lead to increased costs, unneeded treatments, worse outcomes, and may cause you to unnecessarily worry about something that’s normal or inconsequential.
Summary
In summary, there are 5 common myths about MRIs and x-rays:
Myth #1: Imaging Shows The Cause Of Pain
- Fact #1 is that many of these so-called “abnormalities” are actually quite common in people without symptoms, and may be considered normal, age-related changes (similar to wrinkling of your skin or graying of your hair).
Myth #2: Imaging Predicts Your Outcomes
- Fact #2 is that imaging doesn’t necessarily determine your fate, especially if it doesn’t match your current symptoms and function.
Myth #3: If You Fix The Image, You Fix The Pain
- Fact #3 is that we can’t or don’t always need to find something to fix because we’re not machines, but many conditions heal or get better on their own because we are adaptable human beings.
Myth #4: Imaging Dictates Rehab
- Fact #4 is that you, the person, influence the rehab process more so than a single, zoomed-in picture of your anatomy.
Myth #5: Imaging Never Matters
- Fact #5 is that imaging does matter sometimes, but when not used or explained appropriately, it can lead to higher costs and worse outcomes.
Looking to improve your strength, mobility, and overall fitness? Check out our Low Back Resilience program!
Do you want to read other similar blogs? Check out these topics:
Placebo, Training Around Injuries, ACL Surgery
Thanks for reading. Check out the video and please leave any questions or comments below.