The purpose of this blog is to provide a VERY brief review of sacroiliac joint (SIJ) dysfunction assessment and management, unrelated to pregnancy or trauma.
Do you have new, lingering, or recurring low back pain that’s stopping you from doing the things you enjoy or keeping you from feeling like yourself? Check out our Low Back Resilience Program!
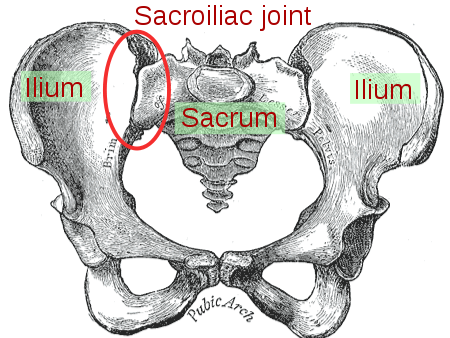
The Sacroiliac Joints (SIJs)
Commonly referred to as the pelvis, the sacroiliac joint(s) is the articulation, or connection between the sacrum and ilia of the innominate bones. Due to its structural integrity and the surrounding muscles, ligaments, and other connective tissues, the sacroiliac joint (SIJ) serves to support the trunk and upper extremities, as well as transfer load between the legs and spine [12]. Vleeming and colleagues characterize it as an amphiarthrotic joint (slightly movable) as it has elements of a synarthrosis (a skull suture is one example) and diarthrosis, or synovial joint (the glenohumeral joint is one example although it is quite mobile) [12]. Since it is able to rotate about and translate along three axes of motion, it is considered to have six degrees of freedom [3]. Not only does the SIJ exhibit anatomical differences between sexes and as we age, there is a large degree of variability between and within individuals [12].
Sacroiliac Joint Assessment
When it comes to the assessment of symptoms in this region, three types of tests are commonly utilized: pain provocation, motion palpation, and pelvic position [10]. The most often used and referenced provocative tests during the clinical examination are the Cluster of Laslett, studied by Laslett et al in 2005 [5]. These tests were introduced to help implicate the SIJ as a contributor to a person’s pain experience. A few years later in 2008, Laslett refined the algorithm for these tests to further assist in ruling in or ruling out the SIJ, without involvement from the low back [6]. Considering that the joint is highly innervated, it is accepted that sensivity in local tissues can contribute to the perception of pain [12].
The word contribute is used twice here strategically as Laslett originally referred to these provocative tests being able to “identify the SIJ as the pain generator” in his seminal paper [5]. However, with the plethora of research currently at our fingertips, we now understand that pain is better described as an experience influenced by many factors rather than having a simple linear correlation with tissue damage.
Sacroiliac Joint Dysfunction
After the provocative tests are deemed positive by physical therapists or other rehab practitioners, the standard route of care involves assessing symmetry in pelvic alignment, or lack thereof, and dynamic testing to objectify aberrant movement [2,4]. Once identified, it is commonplace to employ a strategy that aims to correct these various functional impairments [1]. Therefore, the treatment algorithm is as follows: implicate the SIJ as the source of pain through provocative tests, identify the associated dysfunctions, and fix these abnormalities for symptom resolution.
Reliability of Sacroiliac Joint Tests
Before we even get to treatment, we need to determine just how useful these tests are in identifying these deviations at the pelvis. Can we accurately pinpoint asymmetries in motion and posture? It turns out, in fact, that we cannot. Reviews by van der Wurff and Stovall show us that these tests are unreliable and invalid for their previously described purposes in the management of SIJ related issues [6,8,9]. This is not a knock on the skills of clinicians. The SIJ rotates just a few degrees and moves only millimeters in all directions when measured in people using radiostereometric analysis, the consensus gold standard for accurately quantifying movement in this region [3]. We cannot be expected to feel or see these miniscule changes. Expanding on this topic, it also makes sense then that manipulation of the SIJ doesn’t actually alter joint positioning [9].
Management and Future Direction
If we cannot mobilize or stabilize the SIJ due to its inherent anatomical characteristics, it stands to reason that our treatment choices don’t really matter because the joint isn’t being altered in any significant way, right? Yes and no. Anything can work, and that is where the beauty actually lies. It allows for infinite possibilities, but should be applied within the context of the interventions that will provide the most value in the long run: education and exercise [7]. Education should consist of reassurance that function can improve with the right plan of care and appropriate time frame, and discussions around recognizing and modifying factors that might be contributing to their current symptoms or limitations.
With respect to exercise, the goal should be to improve the capacity and tolerance of the entire person and grade it toward returning to meaningful activities. Things that load the region include squats, deadlifts, lunges, planks, side planks, bridges, hip thrusts, and the list goes on forever. However, the key is utilizing movements that pertain to the person’s goals, finding an entry point, and gradually building up over time.
A Quick Example
A trail runner takes a misstep during one of their training sessions that now limits them from performing any single limb stance, including walking, without experiencing symptoms. The first step might entail having the runner initially swap out running for a different form of cardio to maintain fitness while minimizing aggravation to the region (assuming tolerance allows). The next step is developing a plan with the end goal in mind: return to trail running. The biggest challenge will likely be the impact of landing on a single leg. How can we reverse engineer this motion? End stage rehabilitation (aside from actually running) might be single leg bounds. Go backwards from there until an entry point is found. If that happens to be double limb squats, no problem. You’ve identified the start and end points – fill in the gaps by gradually incorporating and progressing walking, running, and single leg work until trail running is resumed.
Don’t forget to check out our Low Back Resilience Program!
Lumbar Imgaing, Disc Herniations, Sciatica Advice
Thanks for reading. Check out the video and please leave any questions or comments below.
References
- Beales D, Hope JB, Hoff TS, Sandvik H, Wergeland O, Fary R. Current practice in management of pelvic girdle pain amongst physiotherapists in Norway and Australia. Man Ther. 2015;20:109–116.
- Byrd E, May S, Marsden J. The sacroiliac Joint: a survey of the current practice in the United Kingdom. Physiotherapy. 2017;103:e26. doi:10.1016/j.physio.2017.11.184
- Goode A, Hegedus EJ, Sizer P, Brismee J-M, Linberg A, Cook CE. Three-dimensional movements of the sacroiliac joint: a systematic review of the literature and assessment of clinical utility. J Man Manip Ther. 2008;16(1):25-38.
- Hodges C, Maxwell B. A time series survey of physical therapist assessment of sacro-iliac joint dysfunction in the United States. Physiotherapy. 2015;101:e579–e580.
- Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of Sacroiliac Joint Pain: Validity of individual provocation tests and composites of tests. Manual Therapy. 2005;10(3):207-218. doi:10.1016/j.math.2005.01.003
- Laslett M. Evidence-Based Diagnosis and Treatment of the Painful Sacroiliac Joint. Journal of Manual & Manipulative Therapy. 2008;16(3):142-152. doi:10.1179/jmt.2008.16.3.142
- Palsson TS, Gibson W, Darlow B, et al. Changing the Narrative in Diagnosis and Management of Pain in the Sacroiliac Joint Area. Phys Ther. 2019;99(11):1511-1519.
- Stovall BA, Kumar S. Anatomical landmark asymmetry assessment in the lumbar spine and pelvis: a review of reliability. PM R. 2010;2(1):48-56.
- Tullberg T, Blomberg S, Branth B, et al. (1998) Manipulation does not alter the position of the sacroiliac joint – a roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976) 23, 1124–1128.
- van der Wurff P, Hagmeijer RH, Meyne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 1: Reliability. Man Ther. 2000;5(1):30-36.
- van der Wurff P, Meyne W, Hagmeijer R. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 2: Validity. Manual Therapy. 2000;5(2):89-96. doi:10.1016/s1356-689x(99)90229-1
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567.