The purpose of this blog is to discuss the health benefits associated with walking, challenging the notion that we need 10,000 steps per day, utilizing walking for rehabilitation, and talking about ways to make it a consistent part of your weekly routine.
Looking for rehab or performance programs? Check out our store here!
Walking for Health
Exercise is healthy for you. This is no secret, right? Then why do 74% of American men and 81% of American women fail to meet physical activity guidelines that recommend at least 150 minutes of moderate-intensity aerobic activity and 2 days of muscle-strengthening per week [1]? Regular physical activity has been associated with positively treating, managing, and/or lowering the risk for cardiovascular disease, type 2 diabetes, anxiety, depression, various cancers, all-cause mortality, and the list goes on [1-4]. Since walking happens to be the most common form of physical activity, can it be used to meet the aerobic activity guidelines to help individuals improve their quality of life, longevity, and overall function [5]?
Do You Actually Need 10,000 Steps Per Day?
The notion that we need 10,000 steps per day to reap the health benefits associated with walking likely derived from a pedometer marketed, sold, and distributed in Japan named Manpo-kei, which translates to “10,000 steps meter” in Japanese [6]. While this attractive, even number seems logical and simple to remember, its initial recommendations were not necessarily based on research. Furthermore, it doesn’t describe the intensity of the steps (slow, moderate, fast), the bout duration or frequency (one long walk vs. several walks throughout the day), or to whom it applies. Therefore, do we all really need to walk 10,000 steps per day?
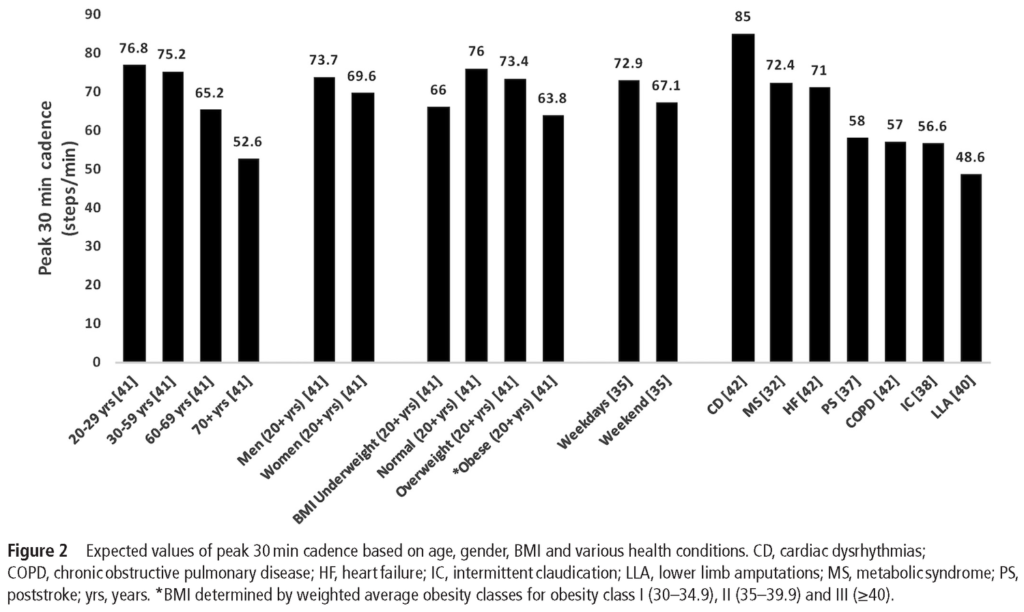
First, let’s consider how much walking is actually required to meet the Physical Activity Guidelines for Americans. Well, moderate-intensity activity is defined as 3.0-5.9 METs (metabolic equivalent of tasks) with brisk walking at roughly 2.5-2.7mph equating to 3 METs [6-7]. Stated another away, walking approximately 100 steps/minute is required for it to be considered moderate-intensity activity [5]. Therefore, only 3-4000 steps over the course of 30 minutes, performed 5 days per week, is needed to meet the physical activity guidelines [6]. However, only 3.6% of US adults average at least 30 min/day of 100 steps/min or more [5]. Additionally, these numbers reflect absolute intensity rather than relative intensity which may not be as suitable for individuals beginning at a lower aerobic capacity such as those who are older or have chronic medical conditions [1].
Moderate-intensity activity is considered to be a 5 or 6 on a 0 to 10 scale where 0 is sitting and 10 is the highest effort possible. It can also be considered physical activity that allows for talking but not singing based on the level of exertion [1]. If we take the absolute or relative intensities into consideration, a person could theoretically hit the recommended dosage of moderate-intensity activity by walking for 30 minutes, 5 times per week, with a 5-6/10 exertion level or at a pace of 100 steps/minute. This differs significantly than the often endorsed 10,000 steps per day, but Tudor-Locke and Bassett 2004 point out that this daily recommendation includes all activity, whereas the 3-4000 steps/day may be a “recommendation to be active ‘over and above’ an undisclosed minimal level of daily activity.”
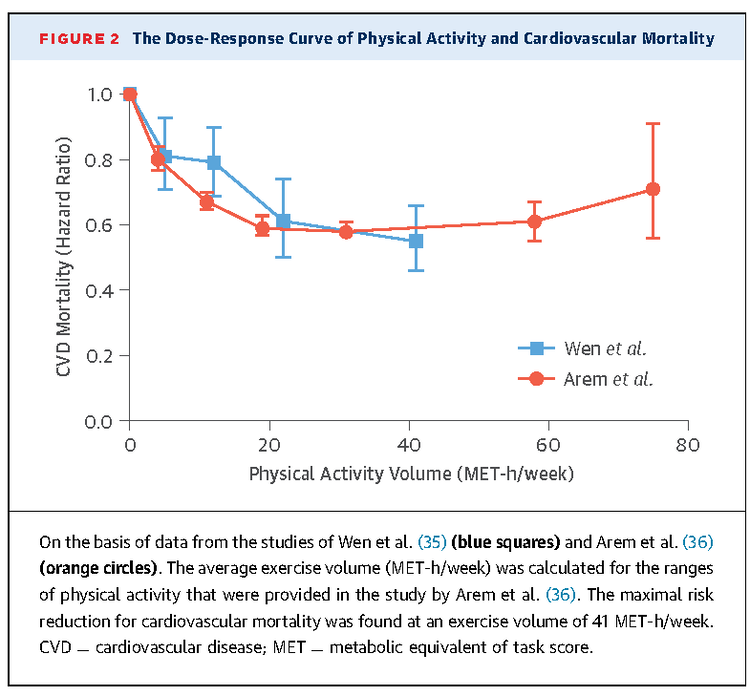
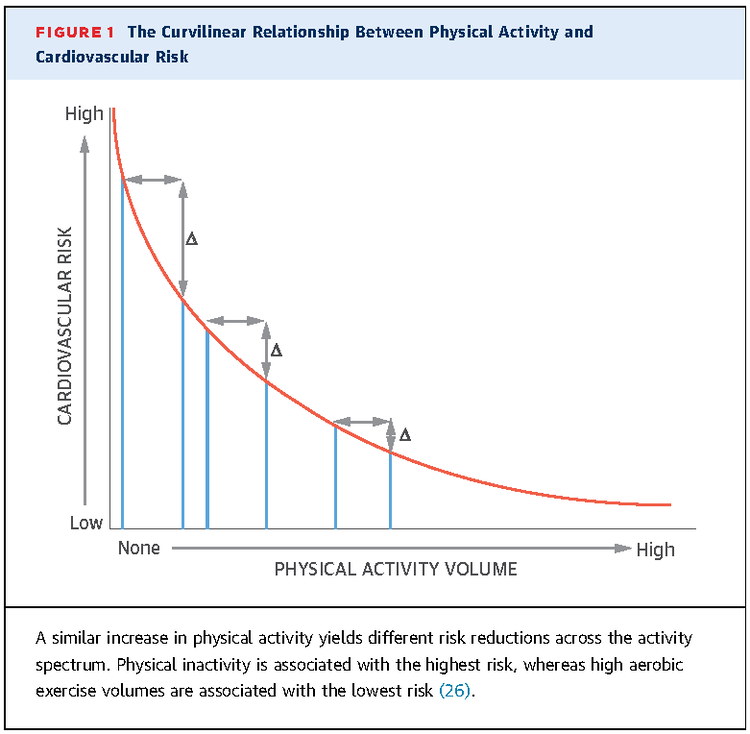
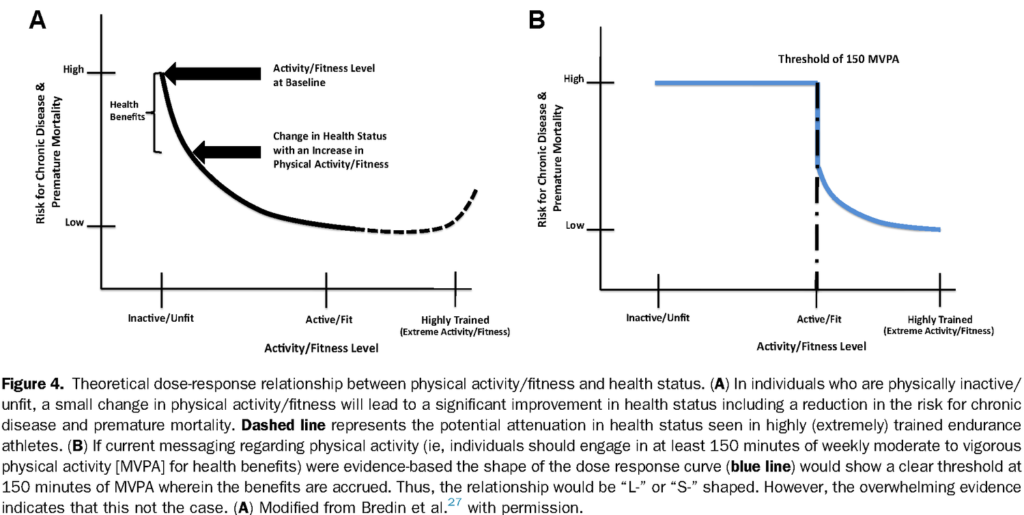
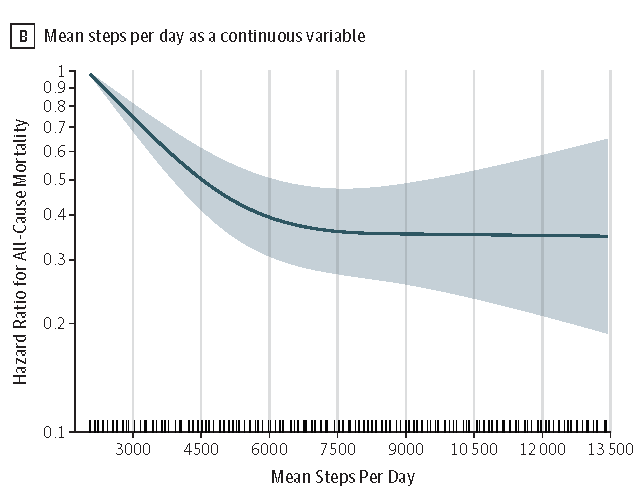
A very important thing to note throughout this discussion is that most physical activity guidelines may be seen as the optimal amount of activity required rather than the minimum needed for health benefits [8]. While the protective effect of exercise does improve with increasing amounts (dose-response relationship), this relationship eventually plateaus likely for a variety of reasons. However, we see that individuals who are inactive or unfit benefit greatly from fairly small increases in activity [9]. This relationship has been written about extensively by Warburton and colleagues [7-9] and can be visualized in the figure below (additional figures at the end). For example, as little as 15 minutes of exercise per day has been associated with a reduction in all-cause mortality by 14% (additional 4% for every additional 15 minutes up to 100 minutes) with the greatest effects being observed within the first 1-2 hours of exercise each week [9].
This information is not suggesting that we should not aim for the recommended level of physical activity laid forth in the guidelines, but it highlights that some exercise is always better than little to no exercise, especially for individuals who are currently inactive, older, or present with other chronic health conditions. The recommendation to exercise at least 150 minutes per week at a moderate intensity can actually serve as a barrier to participation for certain people (more on this in a bit). We also know that physical activity does not have to be continuous, meaning that you can choose to engage in brisk walking for 30 minutes, 10 minutes, or even 2 minutes at a time while still achieving health benefits [1]. Just to hammer this point home, let’s briefly discuss three studies examining the relationship between walking and positive health outcomes.
In 2019, a prospective study by Lee et al. showed that older women (mean age of 72) who walked more steps per day had progressively lower mortality rates until this association leveled off at roughly 7,500 steps/day (figure below). The researchers also found drastic reductions in the mortality rate (41%) for women who walked 4400 steps/day compared to those who walked just 2700 steps/day. Step volume rather than step intensity seemed to be the more important factor in this study [10]. Therefore, we see that walking far less than 10,000 steps per day may be incredibly healthy for older women.
In a prospective study by Jefferis et al. in 2019, authors examined how sedentary behavior and physical activity impact cardiovascular disease onset in older men with a mean age age of 78.4. The researchers found that each increase of 1000 steps/day or each 10 minutes/day increase in moderate to vigorous physical activity were associated with reductions in cardiovascular disease risk by 14% and 11% respectively. It also did not matter if physical activity was accumulated sporadically, such as with 1 minute bouts, or performed continuously for greater than 10 minutes at a time [11].
Lastly, Yates and colleagues in 2014 assessed prospective data to determine if a change in ambulatory activity would alter the risk of a cardiovascular event in individuals with impaired glucose tolerance who were already at a higher risk for a cardiovascular event. Unsurprisingly, the authors concluded that “baseline ambulatory activity and change in ambulatory activity between baseline and 12 months were significantly and inversely associated with the risk of a cardiovascular event”. For example, “each 2000 step increase or decrease in daily ambulatory activity from baseline to 12 months was associated with an additional 8% lower or higher cardiovascular event rate” [12].
Walking for Rehabilitation
The takeaway so far is that walking works for improving health outcomes, but can it utilized for rehabilitation? Analyzing the topic from a broader perspective, a systematic review by O’Connor et al. in 2015 determined that walking can be used as an adjunct for reducing pain in the short and medium terms while improving function long-term in individuals who have chronic musculoskeletal pain [13]. Since persistent musculoskeletal pain is a multi-factorial experience that can negatively affect activities of daily living and participation in work or recreational activities, it’s important to consider how walking may positively impact physical function, as well as things like sleep, depression, and anxiety.
Walking also fares well when compared directly to other interventions. For example, a systematic review by Roddy and colleagues in 2005 found that aerobic walking and home based strengthening exercises were effective at reducing pain and disability in individuals with knee osteoarthritis, but no difference between the two was established in terms of superiority [14]. Similarly, a randomized controll trial by Shnayderman et al. in 2013 found that a six week aerobic walking program was just as effective as six weeks of specific strengthening exercises for chronic low back pain [15]. There’s also a trend for improvement using Nordic walking for chronic low back pain as determined by a single blind randomized clinical trial by Hartvigsen and colleagues in 2010 [16]. Finally, a randomized crossover trial by Riel et al. in 2018 determined that walking fared no worse than isometric or isotonic exercises for altering pain acutely in individuals diagnosed with plantar fasciopathy [17]. In this last study, walking took far less time and instruction which may have important implications for the next section.
Breaking Barriers
If walking is beneficial for rehabilitation and overall health, why do we see less than 27% of American adults meeting the physical activity guidelines? There is no simple answer to this question and this discussion could have its very own blog, but we’re going to do our best to explore some actual or perceived barriers to walking, or just physical activity in general.
Although there are many commonalities across various groups of people, barriers to physical activity may differ based on age, health status, gender, geographical location, beliefs, etc. For example, situational barriers (time, lack of sidewalks, having a lot to carry) and the consideration of personal appearance (ruining nice clothing or hairstyle, restrictive clothing, etc.) are limitations to unstructured and spontaneous walking in college students [18]. In a cohort of adults from a town in Canada, the most barriers to walking were reported by females, senior citizens, and those with high BMI, often secondary to safety, appearance, lack of social support, and time [19].
There are arguably even more barriers to physical activity for individuals experiencing chronic musculoskeletal pain. After performing a systematic review of the literature, Kanavaki and colleagues categorized barriers into physical, psychological, and social-environmental factors for individuals with knee and hip osteoarthritis [20]. Physical health barriers included pain, fatigue, stiffness, limited energy, sense of limited physical capacities, old age, and lack of physical fitness. Psychological factors included components such as the belief that exercise wasn’t helpful or even harmful, previous negative experiences, a sense of boredom or laziness toward exercise, and distress. Social-environmental factors consisted of things like poor communication and support from health professionals, comparing themselves to others, cost, limited accessibility, cold weather, and safety [20].
People with persistent low back pain report similar barriers to physical activity such as lack of time, lack of perceived benefit, no clear diagnosis, kinesiophobia, anticipatory anxiety, lack of motivation, family members encouraging rest, and inappropriate education from healthcare providers [21,22]. Whether low back pain is acute or chronic, each individual’s decision will be influenced by the perceived benefits and risks, as well as various contextual factors [23]. The choice to rest or remain active because of, or in spite of low back pain can be visualized in the figure by Darlow et al. below.
Walking for Health and Rehab Summary
Just as there are barriers to physical activity, there are a plethora of facilitators as well. Many people regularly exercise for the physical, psychological, or perceived benefits that exercise affords. For individuals in pain, it may be more important to encourage exercise based on its psychological and social benefits as they are often seen as more important than the physical benefits. It’s also important to focus on the positive aspects of exercise rather than dwelling on the negative impact of inactivity [23]. Like the barriers to physical activity though, the facilitators will be different for each individual so it might be vital to ask others, or yourself, what can be done to make exercise more manageable, meaningful, and memorable.
Key Takeaways for Walking
- The Physical Activity Guidelines for Americans suggest that individuals should aim for at least 150 minutes of moderate-intensity aerobic activity and 2 days of muscle strengthening per week, yet 74% of American men and 81% of American women fail to meet these guidelines.
- Walking is the most common form of exercise and may be one of the best ways to achieve 150 minutes of moderate-intensity aerobic activity each week. Speaking in terms of absolutely intensity, this can be accomplished by walking at roughly 2.5-2.7 mph, or 100 steps/min, for 30 minutes per day which equates to 3-4000 steps of dedicated exercise. With respect to relative intensity, aim for 30 minutes, 5 days per week, at an effort of 5 to 6 on a 0 to 10 scale.
- Despite popular belief, people don’t necessarily need to achieve 10,000 steps per day to reap health benefits. In fact, individuals who are less active, older, or present with other chronic medical conditions may see large benefits with just small increases in activity. Additionally, physical activity can be sporadic throughout the day rather than having to be completed during set blocks of time. Some activity is better than no activity, and it doesn’t matter if you accomplish that in 2 minute increments or 30 minute bouts.
- Walking can be useful for musculoskeletal rehabilitation as demonstrated in individuals with low back and knee pain. Walking does not necessarily have to be done as a replacement to more traditional treatments or exercise, but can be seen as an adjunct (although it can act as a stand-alone intervention if you so choose). Walking has various physical and psychological benefits that may aide in the management of acute or chronic musculoskeletal pains.
- Common barriers to physical activity include time, safety, and perceived risks so it’s important to determine what’s realistic and meaningful to you. It can be helpful to discuss a plan with your healthcare provider.
- If I were to suggest my preferred form of walking, it would be outdoors without the use of a cellphone for its potential positive impact on mental health outcomes such as depression and anxiety [24]. Outdoor walking groups, or simply having a walking buddy, can also serve as a way to influence adherence in a positive manner [25]. Start small, set goals, and try to make it habitual and enjoyable.
Looking to improve your knee strength, range of motion, and power to enhance your function and performance? Check out our Knee Resilience program!
Want to learn more? Check out some of our other blogs:
Sleep, Peroneal Tendinopathy, Hip Bursitis?
Thanks for reading. Check out the video and please leave any questions or comments below.
References
- Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi:10.1001/jama.2018.14854
- Luan X, Tian X, Zhang H, et al. Exercise as a prescription for patients with various diseases. Journal of Sport and Health Science. 2019;8(5):422-441. doi:10.1016/j.jshs.2019.04.002
- Kelly P, Williamson C, Niven AG, Hunter R, Mutrie N, Richards J. Walking on sunshine: scoping review of the evidence for walking and mental health. Br J Sports Med. 2018;52(12):800-806.
- Eijsvogels TMH, Molossi S, Lee D-C, Emery MS, Thompson PD. Exercise at the Extremes: The Amount of Exercise to Reduce Cardiovascular Events. J Am Coll Cardiol. 2016;67(3):316-329.
- Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 2018;52(12):776-788.
- Tudor-Locke C, Bassett DR. How Many Steps/Day Are Enough? Sports Medicine. 2004;34(1):1-8. doi:10.2165/00007256-200434010-00001
- Warburton, D.E., Charlesworth, S., Ivey, A. et al. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act 7, 39 (2010). https://doi.org/10.1186/1479-5868-7-39
- Warburton, Darren & Bredin, Shannon. (2016). Reflections on Physical Activity and Health: What Should We Recommend? Canadian Journal of Cardiology. 32. 10.1016/j.cjca.2016.01.024.
- Warburton DER, Bredin SSD. Lost in Translation: What Does the Physical Activity and Health Evidence Actually Tell Us? Lifestyle in Heart Health and Disease. 2018:175-186. doi:10.1016/b978-0-12-811279-3.00013-6
- Lee I-M, Shiroma EJ, Kamada M, Bassett DR, Matthews CE, Buring JE. Association of Step Volume and Intensity With All-Cause Mortality in Older Women. JAMA Intern Med. May 2019. doi:10.1001/jamainternmed.2019.0899
- Jefferis BJ, Parsons TJ, Sartini C, et al. Does total volume of physical activity matter more than pattern for onset of CVD? A prospective cohort study of older British men. International Journal of Cardiology. 2019;278:267-272. doi:10.1016/j.ijcard.2018.12.024
- Yates T, Haffner SM, Schulte PJ, et al. Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. The Lancet. 2014;383(9922):1059-1066. doi:10.1016/s0140-6736(13)62061-9
- O’Connor SR, Tully MA, Ryan B, et al. Walking exercise for chronic musculoskeletal pain: systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96(4):724-734.e3.
- Roddy E, Zhang W, Doherty M. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Annals of the Rheumatic Diseases. 2005;64(4).
- Shnayderman I, Katz-Leurer M. An aerobic walking programme versus muscle strengthening programme for chronic low back pain: a randomized controlled trial. Clin Rehabil. 2013;27(3):207-214.
- Hartvigsen J, Morsø L, Bendix T, Manniche C. Supervised and non-supervised Nordic walking in the treatment of chronic low back pain: a single blind randomized clinical trial. BMC Musculoskelet Disord. 2010;11:30.
- Riel H, Vicenzino B, Jensen MB, Olesen JL, Holden S, Rathleff MS. The effect of isometric exercise on pain in individuals with plantar fasciopathy: A randomized crossover trial. Scand J Med Sci Sports. 2018;28(12):2643-2650.
- Dunton GF, Schneider M. Perceived barriers to walking for physical activity. Prev Chronic Dis. 2006;3(4):A116.
- Clark AF, Scott DM. Barriers to Walking: An Investigation of Adults in Hamilton (Ontario, Canada). Int J Environ Res Public Health. 2016;13(2):179.
- Kanavaki AM, Rushton A, Efstathiou N, et al. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open. 2017;7(12):e017042.
- Boutevillain L, Dupeyron A, Rouch C, Richard E, Coudeyre E. Facilitators and barriers to physical activity in people with chronic low back pain: A qualitative study. PLoS One. 2017;12(7):e0179826.
- Slade SC, Patel S, Underwood M, Keating JL. What are patient beliefs and perceptions about exercise for nonspecific chronic low back pain? A systematic review of qualitative studies. Clin J Pain. 2014;30(11):995-1005.
- Darlow B, Perry M, Dean S, Mathieson F, Baxter GD, Dowell A. Putting Physical Activity While Experiencing Low Back Pain in Context: Balancing the Risks and Benefits. Arch Phys Med Rehabil. 2016;97(2):245-251.e7.
- Kelly P, Williamson C, Niven AG, Hunter R, Mutrie N, Richards J. Walking on sunshine: scoping review of the evidence for walking and mental health. Br J Sports Med. 2018;52(12):800-806.
- Hanson S, Jones A. Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. 2015;49(11):710-715.