Should you always avoid pain when exercising? Is there a perfect posture? Which exercises are bad for you? The purpose of this blog is to debunk the 7 most common exercise and rehab myths!
Looking for rehab or performance programs? Check out our store here!

Myth #1: Imaging Shows The Cause of Pain
Let me tell you 2 facts about imaging:
1. Structural “abnormalities” found by x-rays or MRIs are actually quite common in people without symptoms.
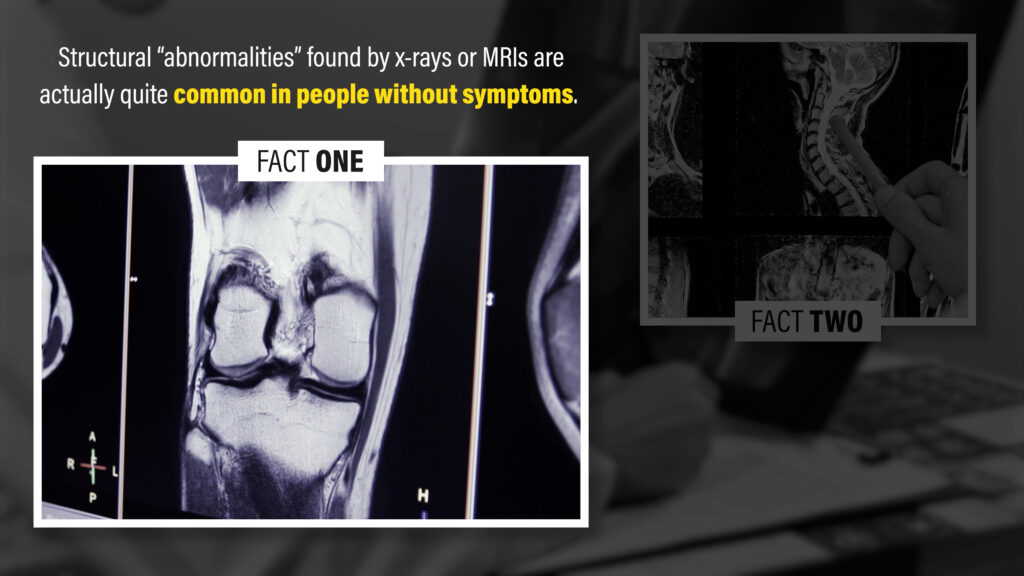
For example, a study by Horga et al in 2020 had 115 uninjured adults undergo imaging of their knees and concluded that “nearly all knees of asymptomatic adults showed abnormalities in at least one knee structure on MRI,” including 30% presenting with meniscal tears.
What if you do have pain? Well, a study by Barreto et al in 2019 evaluated 123 individuals who had one-sided shoulder pain and concluded that “most abnormal MRI findings were not different in frequency between symptomatic and asymptomatic shoulders.”
2. Surgically “fixing” or removing an abnormality doesn’t guarantee the elimination of symptoms, and often doesn’t fare better than non-surgical management.
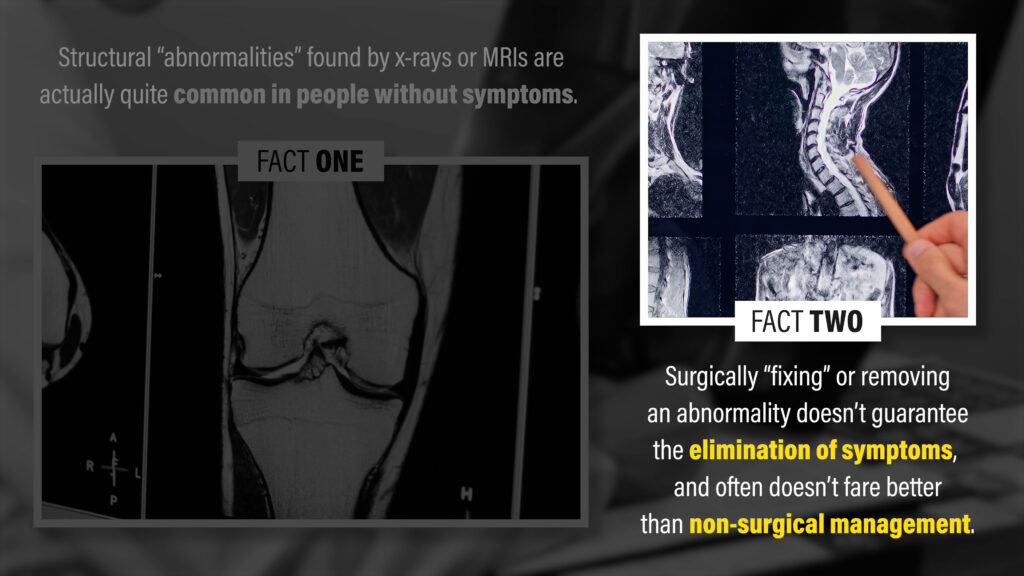
For example, a systematic review by O’Connor et al in 2022 concluded that arthroscopic surgery for degenerative meniscal tears “provides little or no clinically important benefit in pain or function.. and may not improve treatment success compared with a placebo procedure.”
Sometimes imaging does matter because of its correlation with your symptoms or function, but there’s often too much of an emphasis placed on x-rays and MRIs. If you’re trying to find a connection between your imaging findings and symptoms, it’s usually not hard to do so.
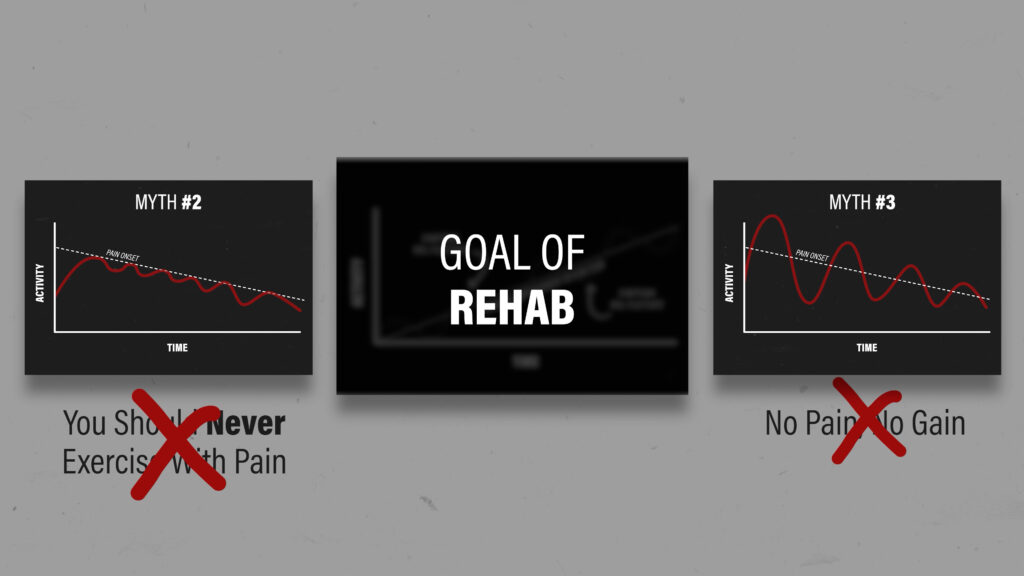
Myth #2: You Should Never Exercise With Pain
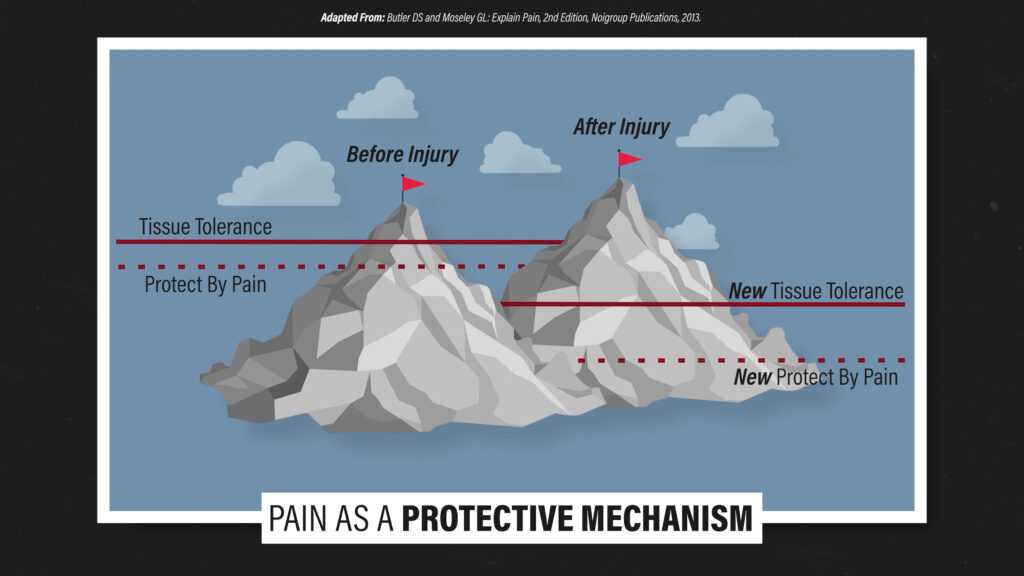
Since imaging findings don’t always correlate with your symptoms, pain doesn’t always equate to tissue damage. In some cases, pain serves as a protective mechanism – it occurs prior to tissue damage.
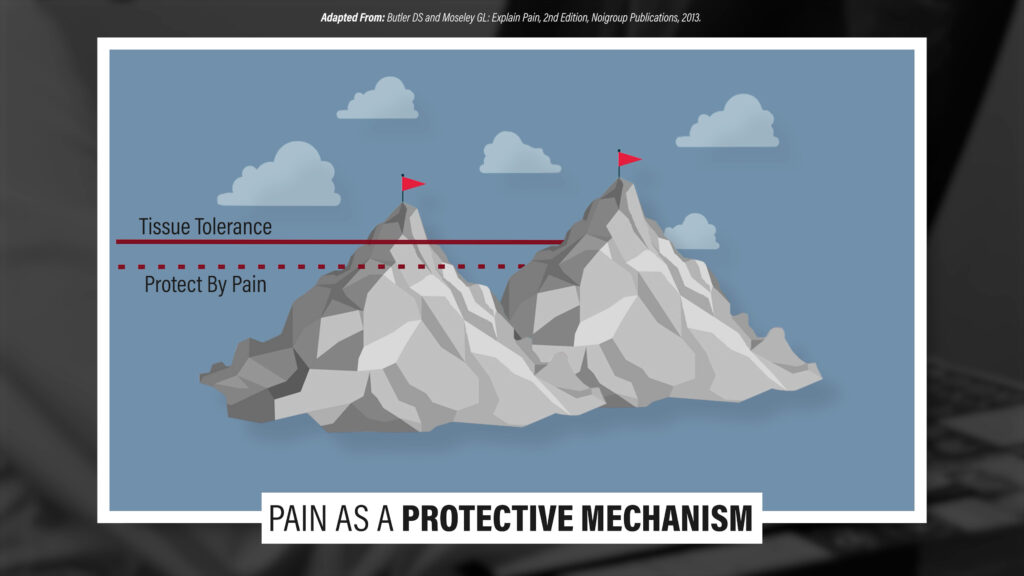
Bend your finger backward within tolerance. It hurts, but when you let go, the pain goes away and no damage occurred. Or think about the last time you turned up the hot water in the shower too quickly. It stung, but you didn’t truly get hurt.
A study by Hickey et al in 2020 split athletes with acute hamstring strains into 2 groups. One group was asked to perform and progress all exercises while remaining completely pain-free. The other group was allowed to perform and progress exercises up to a 4/10 pain. They found that both groups returned to sport within a similar time frame and had the same number of reinjuries 6 months later.
If you consider that most tissues heal within a few months of an initial injury, including broken bones, the idea that you should never exercise with pain makes less sense as symptoms become more chronic in nature.
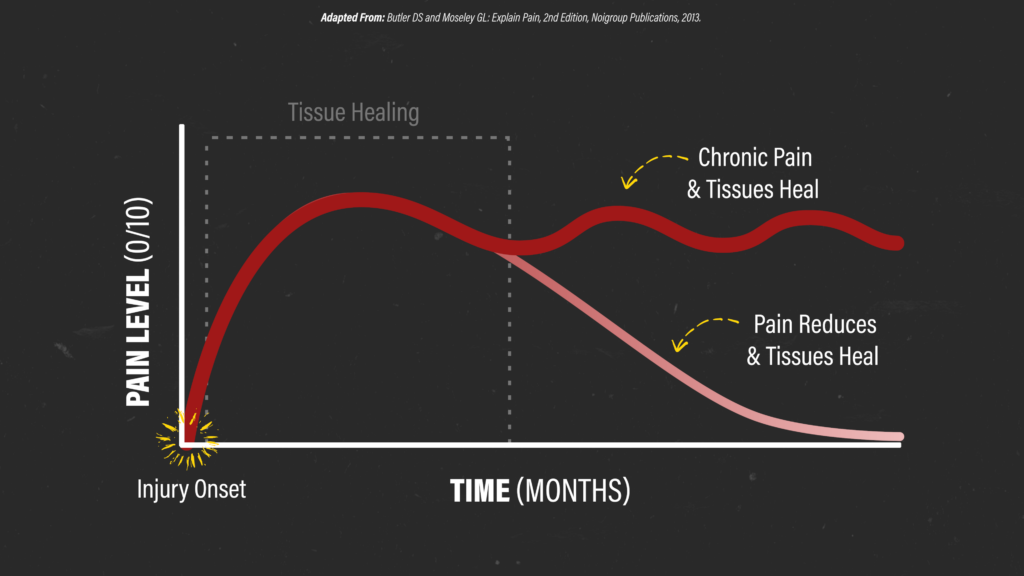
If you’ve had pain for 2 years, it’s possible that your sensitivity has increased despite healing having occurred, but it doesn’t necessarily mean you’re damaging anything.
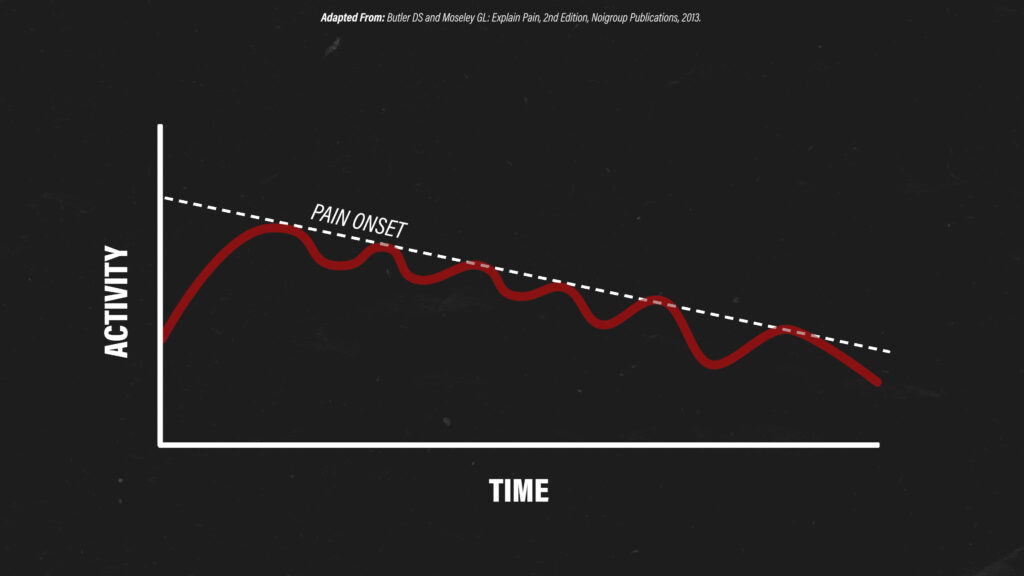
If you have pain at rest or with any form of exercise, but you try to wait until you’re completely pain-free to start exercising, you might end up doing less and less until you’re not exercising at all.
Myth #3: No Pain, No Gain
Just because pain doesn’t always mean that you’re causing harm, doesn’t necessarily mean that you should purposely be pushing into significant pain. In certain scenarios, like immediately after fracturing your ankle, you’re not going to ignore those symptoms and hop around on that leg. Most examples aren’t this extreme, though.
In reality, for some people who try to push through pain, they may cause a flare-up that requires a period of rest to allow that spike in symptoms to subside. If they choose to continually repeat this process, they end up getting worse instead of better. They’re taking 2 steps backward for every step forward.
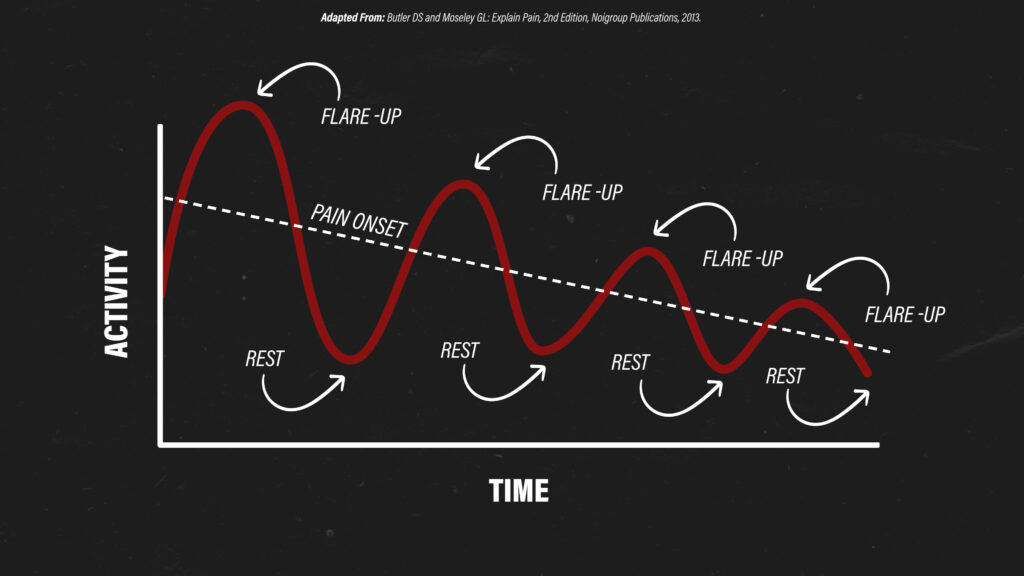
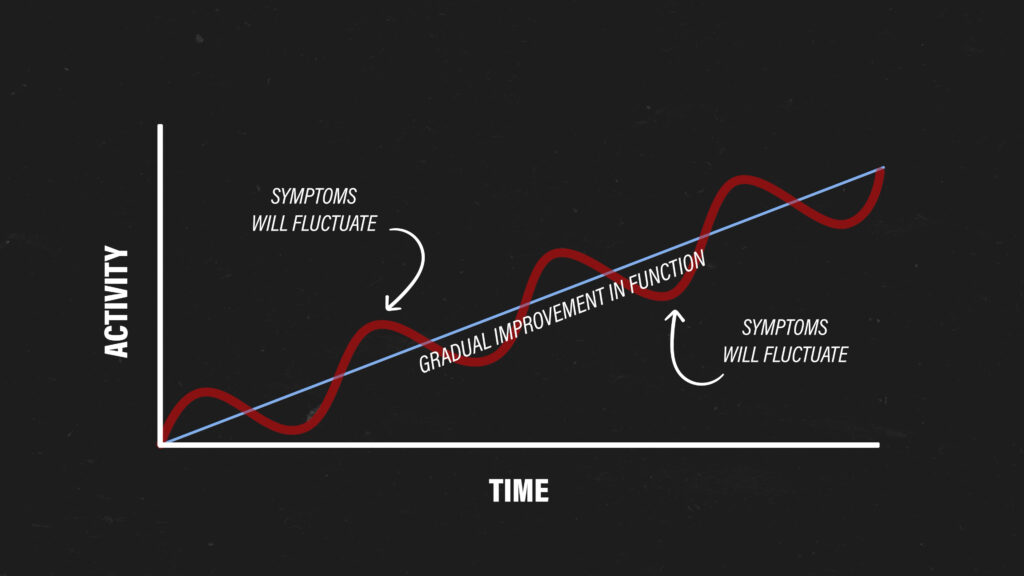
Rehab is usually about trying to find a balance between myths #2 and #3. You rarely need to completely rest and avoid all symptoms, but you also shouldn’t approach rehab with a “no pain, no gain” mentality.
Ups and downs are expected, but if your symptoms are tolerable during exercise, you’re minimizing flare-ups, and you’re gradually working toward your goals, you’re probably moving in the right direction.
The rest of the myths are usually presented as very black and white, but each one has way more than 50 shades of gray.
You might not completely agree with me, which is fine, but hopefully you’ll leave this blog with the understanding that these topics are much more complex than what they’re usually made out to be.
Myth #4: There’s A Perfect Posture
Which posture is better between these two?
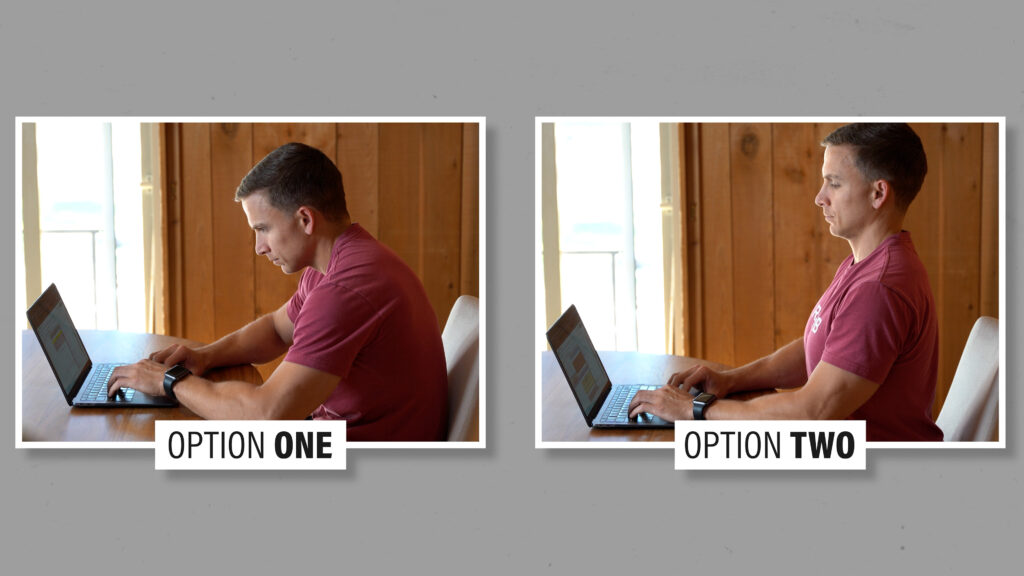
What about now?

And now?

Last one.
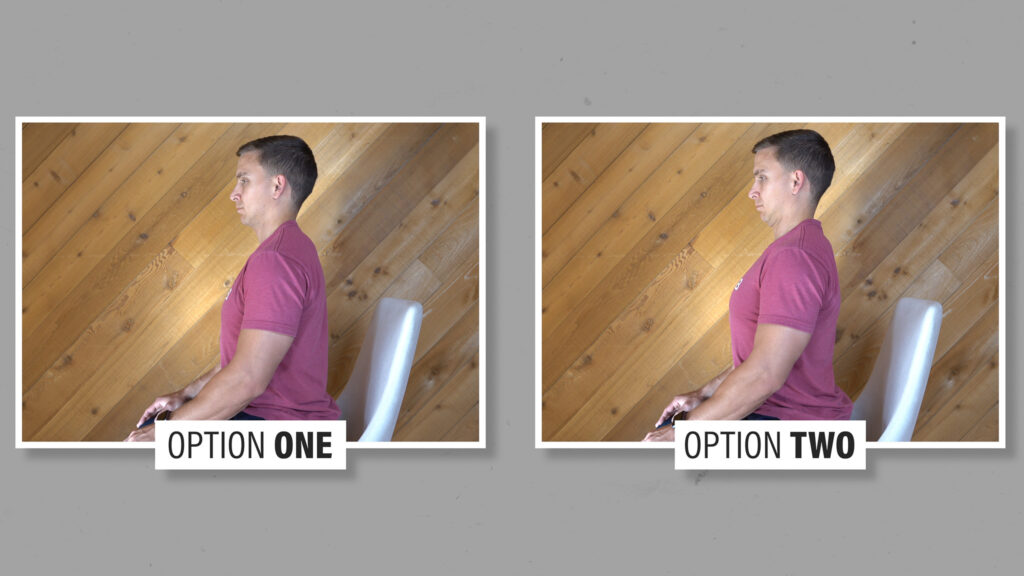
Which postures did you choose? Why? What makes a posture “good” or “bad”?
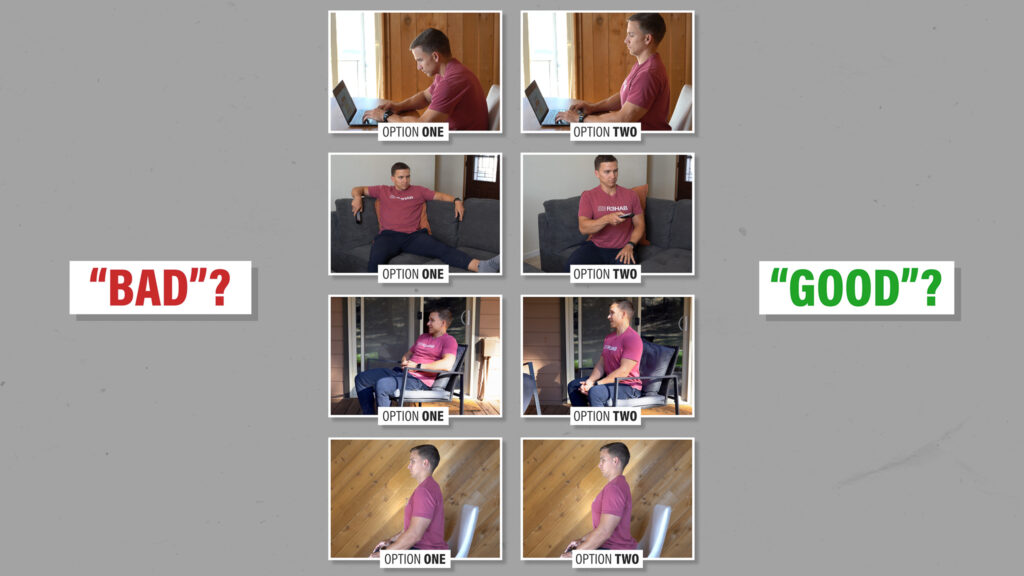
Is the “bad” posture the one most associated with pain? If that’s the case, consider a study by Grob et al in 2007 that found “no association between the sagittal alignment of the cervical spine (or its individual segments) and the presence of neck pain.”
Is the “bad” posture the one most likely to cause pain in the future? A study by Okada et al in 2009 followed asymptomatic volunteers for 10 years and reported that “there was no significant correlation between the sagittal alignment of [the] cervical spine at the time of the first MRI and the occurrence of clinical symptoms over the next 10 years.”
Is a snapshot of your posture even reproducible? And does it reliably predict how you actually look and move throughout the day?
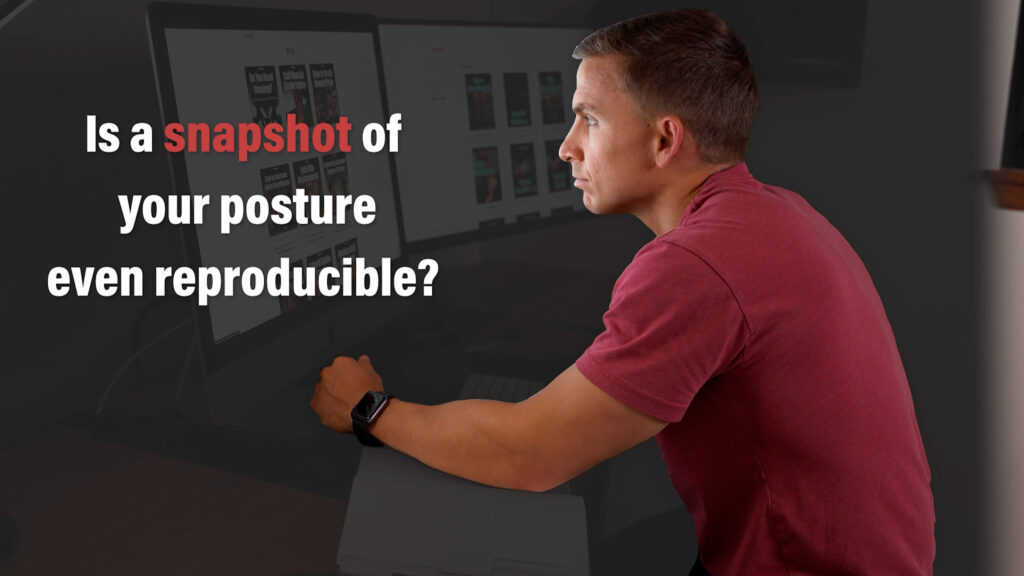
Research would suggest not.

A study by Schmidt et al in 2018 concluded that “standing is highly individual and poorly reproducible.” This is true within individuals and between individuals, whether they’re experiencing pain or not.
A different study by Dreischarf et al in 2016 concluded that the “results of short-term examinations differ considerably from the average values during real-life.”
If you’re seeking help for pain, the person you’re seeing shouldn’t be basing their entire treatment on a snapshot of your sitting or standing posture, or defining success as a change in that snapshot of your posture.
You can have “poor” posture with no neck pain. You can also have “good” posture with significant neck pain. The idea that any one posture is safer or riskier than another is based on years of societal and cultural beliefs as opposed to research.
Does that mean posture never matters? Of course not. I just don’t want you to permanently avoid or obsess over certain postures because you’ve heard that they’re harmful.
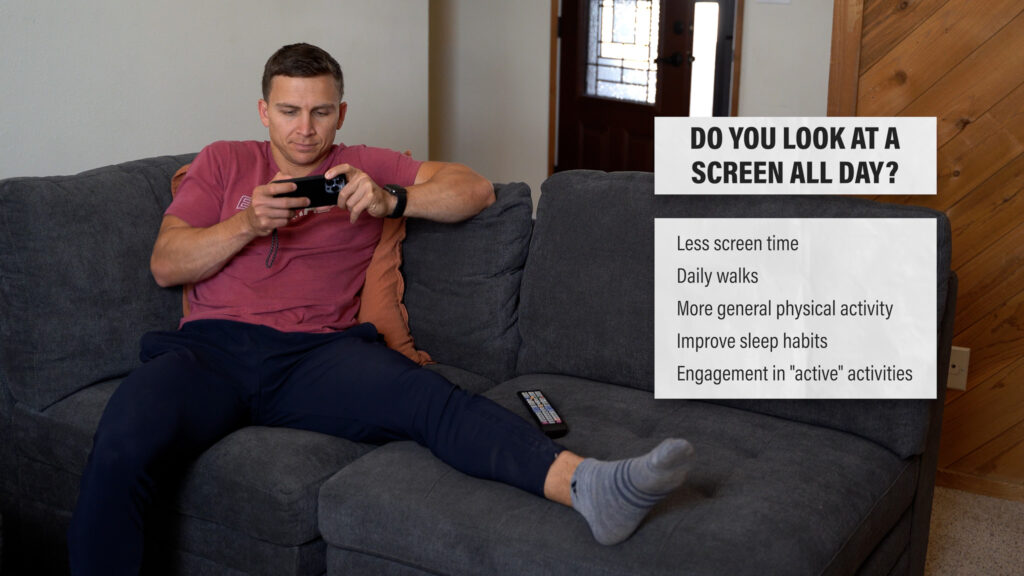
Let’s say you have neck pain with prolonged periods of sitting. Could your symptoms be associated with the position of your neck in sitting? Sure. But they could also be related to a lack of movement and inactivity, the stress of what you’re working on, and a variety of other factors.

A simple solution might be to change your sitting position, stand up for a bit, or go for a walk, without overly stressing about the position of your neck. And, as an example, if you spend 14 hours per day looking at your phone, TV, and computer screen, changing particular aspects of your lifestyle is probably more important than worrying about your posture.
Also, it’s just as possible for someone to experience pain with prolonged periods of standing. Sometimes people actually feel worse trying to stand up straight or sit up tall all the time because they’re trying to avoid sitting or slouching based on the belief that it’s harmful.

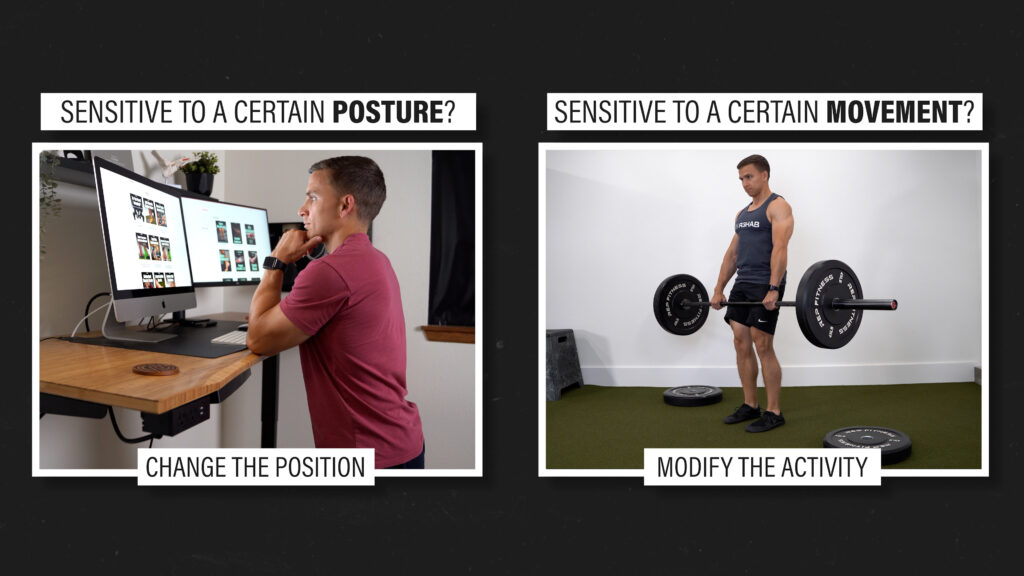
Being sensitive to certain positions or postures doesn’t mean they’re bad or the sole cause of pain. However, if temporarily (or permanently) changing how you interact with your environment makes you feel better, physically or mentally, I’m all for it.
Myth #5: There Are Proper Ways To Move
Based on these two pictures, who do you think is more likely to tear their ACL?

A study by Mørtvedt et al in 2020 informs us that your guess is no better than a coin flip.
Although research by Della Villa et al in 2020 helps us better understand the injury mechanisms, situational patterns, and biomechanics of ACL injuries, “there is currently no screening test available to predict sports injuries.” A study by Arundale et al in 2018 even showed that knee injuries can be reduced with an exercise program that doesn’t actually change how someone moves.
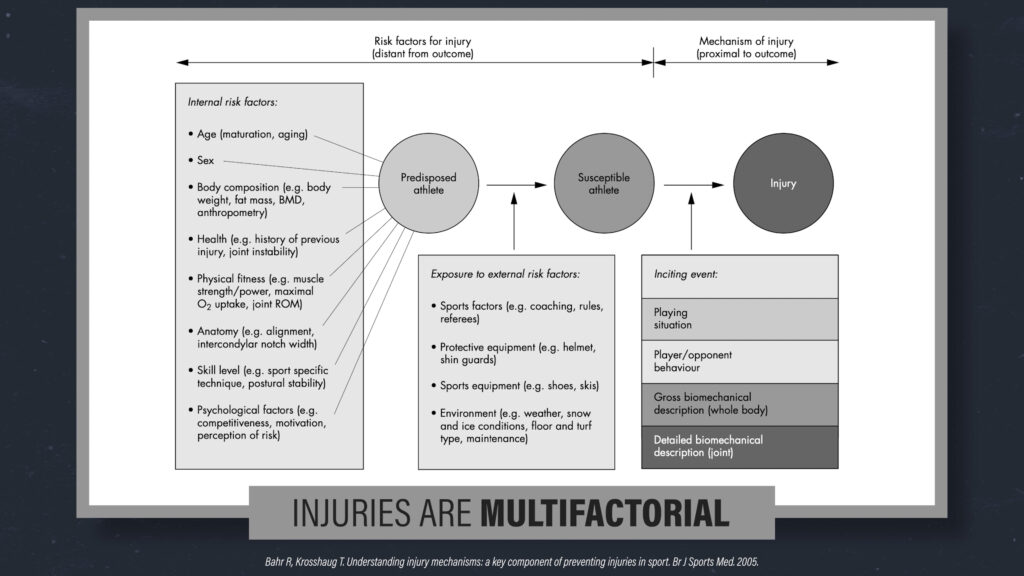
Injuries are multifactorial, and observing how someone moves in a controlled environment is just one small piece of a very large puzzle.
If complex outcomes could always be predicted by simple variables, the NFL Combine numbers would always be associated with the players that go on to have the most success in the league.
Based on these two pictures, who do you think has shoulder pain?

Once again, research by Hickey et al in 2007 tells us that your guess is no better than a coin flip.
If I told you who had symptoms beforehand though, even if they didn’t actually have symptoms, research by Plummer et al in 2017 informs that you’d be more likely to find “problems” with how that person moves. And there’s several studies showing that people can have an improvement in symptoms and function without changing how their shoulder moves.
Like posture, being sensitive to certain positions or movements doesn’t mean they’re bad or the sole cause of pain. If a certain movement or activity exacerbates your symptoms, it’s certainly worth exploring if there are ways that you can modify it.
When it comes to performance, there may be more optimal ways to move on average, but even then, how a body moves best is highly variable. Take Michael Johnson for example. He is one of the fastest runners of all-time despite his unorthodox technique.
It’s advantageous to have more movement options available to you. The best table tennis players in the world have much more variability in how they can hit the ball successfully compared to novices.
You will never even perform the same squat twice. It might look similar, but the execution will always be different. It’s repetition without repetition.
I’ll leave you with one last thing to think about for this section:
There are many different groups, gurus, and schools of thought all claiming to have found the most optimal way to move for injury prevention.
How can this be? Are they all right? All wrong? Or is it possible that there is simply no right or wrong way to move?
Myth #6: You Can Become Bulletproof
Since injuries are so complex, multifactorial, and unpredictable, it’s impossible to completely prevent them. Even a bulletproof vest doesn’t 100% guarantee the prevention of harm or death. Its purpose is to reduce your risk of injury, just like a comprehensive training program.
People who claim to be bulletproof still have pain from time to time. It’s a normal human experience. ”Bulletproof” is just a marketing buzzword used to drive engagement and sales.
Myth #7: There Are Universally Bad Exercises
Since there are no real “best” or “right” ways to move, then it follows that there are also no “wrong” ways to move.
If you scroll through various social media platforms, you’ll find people telling you how not to move, how not to exercise, and how not to perform a given task.
This is a very simplistic way to view exercise and training, and ignores the benefits of movement variability and the importance of individual factors, needs, and goals in exercise prescription and performance.
Leg extensions are a good example of an exercise that people have deemed to be bad because “they put too much stress on your knees.” First of all, squats put just as much stress on your knees as leg extensions, if not more. Second of all, when did stress become a bad thing?
Do you want to improve your cardiorespiratory fitness? Stress your heart and lungs.
Do you want to build muscle? You have to stress your muscles.

Stress isn’t good or bad. It just helps elicit adaptations, one way or the other, based on the stimulus and recovery.
How can you claim that leg extensions are bad without any consideration for sets, reps, frequency, load, range of motion, etc.?
If I try to squat 500lbs and collapse under the bar, is squatting bad?
If I decide to run a marathon without any training and my knee starts to hurt, is running to blame?
Believe it or not, there’s no research to suggest that any exercise is inherently more dangerous than another. Not even upright rows.
If I do one repetition of an upright row with an unweighted dowel, is it bad for my shoulders? What if I do 2 repetitions? What if I do 2 repetitions with 5 pounds? When does it become bad for me?
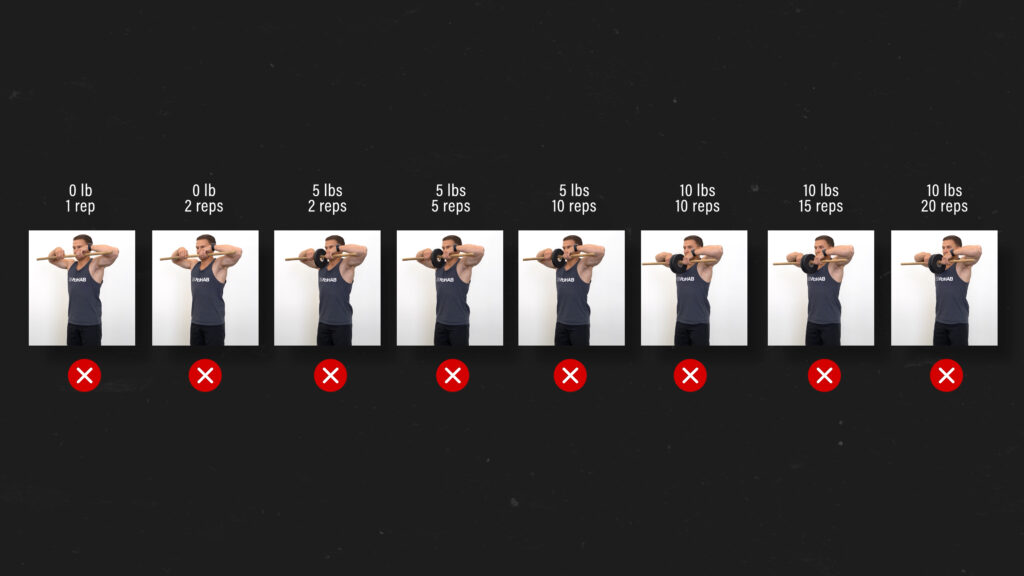
It’s easier to make things black and white for social media, but these kinds of discussions need to be viewed through a critical lens.
And you might be thinking that research isn’t needed because everyone already knows that upright rows are bad for you. But how is that information known?
Well, someone stated it as fact and we all decided it to be true. Kind of like when the Earth was known to be the center of the Universe.
I also know there’s the argument that someone might not have issues with upright rows now, but just wait 20 years. Well, as I already mentioned, no one’s bulletproof. It would actually be unusual for someone to not have at least one episode of shoulder pain over the course of 20 years.
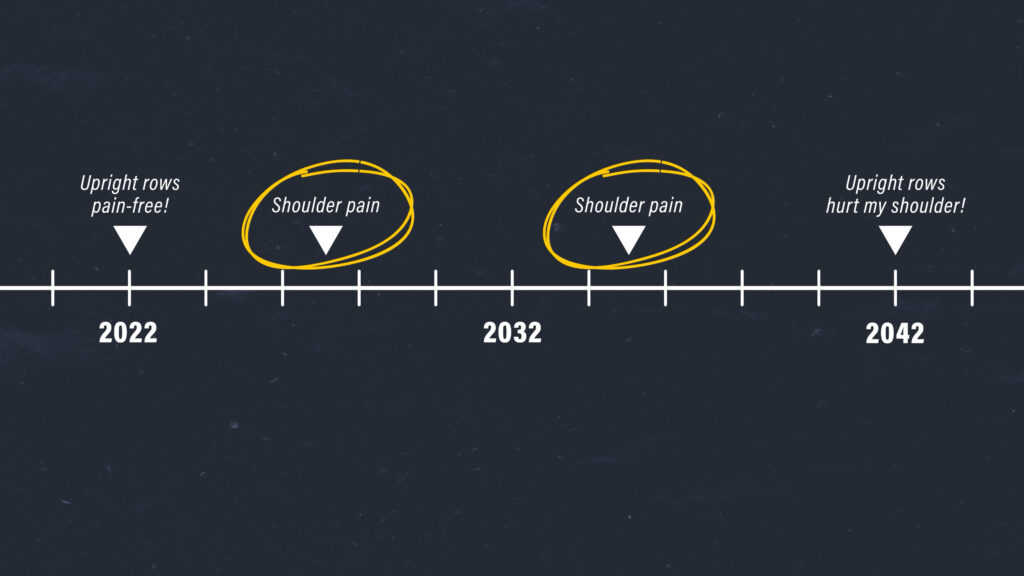
And like I said in Myth #1, it’s easy to find a connection between things if you’re looking for one, especially if your beliefs and expectations have been influenced by what you’ve read or heard over the years.
I’ve never seen someone with shoulder pain due to upright rows, but I’ve seen a lot of people who have pain with walking. I’ve never told any of them that walking is bad for them.
Two final points here:
- I understand that you might have a very strong opinion about the topic based on your experience or understanding, and I’m not trying to take that away from you. I’m just trying to demonstrate that these complex conversations can’t be summarized with a green check mark and red x.
- You don’t have to do any exercise that you don’t want to do. Your exercise choices don’t personally affect me, and I’m not getting paid by “Big Upright Row.”
Exercise and Rehab Myths Summary
In summary, these are 7 of the most common exercise & rehab myths:
Myth #1: Imaging Shows The Cause Of Pain
- Fact #1 is structural “abnormalities” found by x-rays or MRIs are actually quite common in people without symptoms. Imaging does matter sometimes, but it’s often overemphasized. Generally when it comes to imaging, if you’re looking for a connection, you’re going to find it.
Myth #2: You Should Never Exercise With Pain
Myth #3: No Pain, No Gain
- Facts #2 and #3 are that you rarely need to completely rest and avoid all symptoms, but you also shouldn’t approach rehab with a “no pain, no gain” mentality. Ups and downs are expected, but if your symptoms are tolerable during exercise, you’re minimizing flare-ups, and you’re gradually working toward your goals, you’re probably moving in the right direction.
Myth #4: There’s A Perfect Posture
- Fact #4 is being sensitive to certain positions or postures doesn’t mean they’re bad or the sole cause of pain. If changing how you sit or move makes you feel better, physically or mentally, I’m all for it. However, the idea that any one posture is safer or riskier than another is based on years of societal and cultural beliefs as opposed to research.
Myth #5: There Are Proper Ways To Move
- Fact #5 is that similar to posture, we’re unable to predict injuries or the development of symptoms based on how someone moves. The human body is a complex system and how a body moves best, therefore, is highly variable.
Myth #6: You Can Become Bulletproof
- Fact #6 is that pain and injuries are not completely avoidable. Like a bulletproof vest, a comprehensive training program can reduce your risk of injury, but cannot fully guarantee prevention.
Myth #7: There Are Universally Bad Exercises
- Fact #7 is that there are exercises that are more or less appropriate for accomplishing a specific task, but their usefulness cannot be determined without consideration of programming parameters, your training history and goals, etc. There’s also no research to suggest that any one exercise is inherently more dangerous than another.
Looking to improve your knee strength, range of motion, and power to enhance your function and performance? Check out our Knee Resilience program!
Do you want to read other similar blogs? Check out these topics:
Placebo, Training Around Injuries, Imaging Myths
Thanks for reading. Check out the video and please leave any questions or comments below.