The purpose of this blog is to answer some questions about sciatica as it relates to disc herniations. What is sciatica? Are your discs like jelly doughnuts? Can your disc slip? Is your nerve trapped or pinched? Is there a best exercise? Is surgery a good option? If you’re looking for a blog that promises a quick fix, this isn’t it but I hope the information I provide is even more valuable.
Do you have new, lingering, or recurring low back pain that’s stopping you from doing the things you enjoy or keeping you from feeling like yourself? Check out our Low Back Resilience Program!
What is Sciatica?
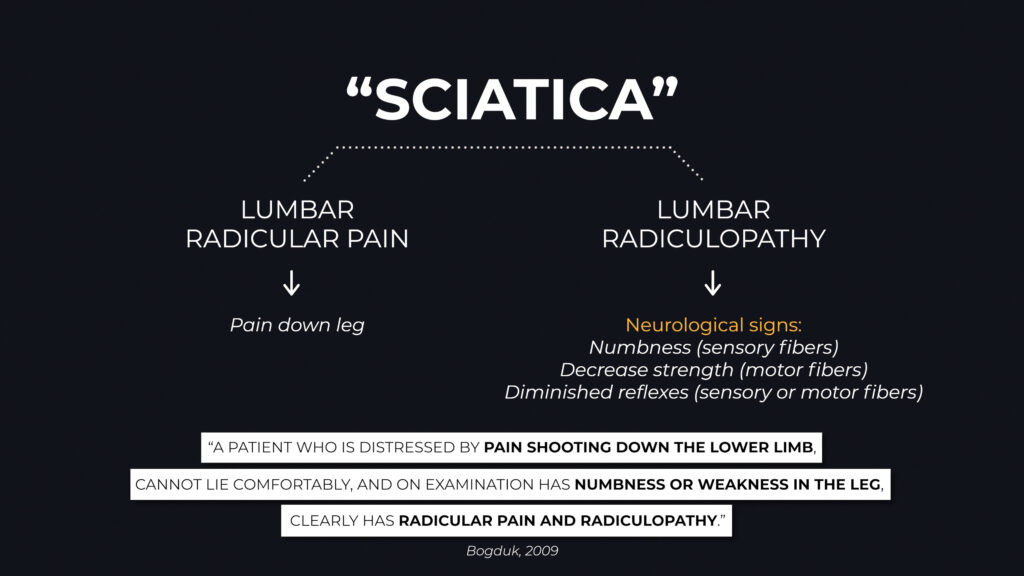
Well, it’s often a catch-all word that people use to describe symptoms down their leg. Individuals might characterize it as pain, burning, numbness, tingling, or whatever descriptor fits what they’re feeling. Sometimes it’s really hard to describe, and these symptoms may or may not coincide with low back pain.
Many people associate “sciatica” with the sciatic nerve because the sciatic nerve travels along the back of the thigh. That’s not quite right, though. The sciatic nerve does travel along the back of the leg, but it’s formed from a bunch of nerves that come together in your low back region. Rather than the symptoms in your leg being caused by irritation of the sciatic nerve, it’s much more common that one of those nerves in the low back is irritated.
Sciatica is somewhat of an ambiguous, umbrella term. In the medical community, if you have pain down your leg that’s associated with an irritated nerve in the low back, that would be called lumbar radicular pain. If you have numbness or a loss of strength because of the same irritated nerve, that’s called lumbar radiculopathy. They’re not exactly the same thing because lumbar radicular pain refers to the pain in the leg whereas lumbar radiculopathy refers to neurological changes like numbness and weakness. But they can often happen together.
For the simplicity of this blog, I’m just going to keep using the word sciatica.
Disc Herniations
Disc herniations are the most common culprit of sciatica and are classified as protrusions, extrusions, and sequestrations. There’s also a different category known as a bulging disk. Once again, for the purpose of the blog, I’m just going to clump everything together as a disc herniation.
To help you understand how a disc herniation can contribute to symptoms in your leg, I want to answer a few questions.
Is Your Disc Like A Jelly Doughnut?
No. This analogy is used because, similar to a jelly doughnut, there’s an outer layer of the disc known as the annulus fibrosus and an inner component known as the nucleus pulposus. The inner layer can push beyond the boundary of the outer layer, but the process isn’t as simple or terrifying as it’s made out to be, and the disc isn’t that fragile. Unlike a jelly doughnut, your discs can resist compression, tension, torsion, etc. They’re strong and adaptable.
In the case of disc herniations, there’s also some good news.
- Systematic reviews by Chiu et al in 2015 and Zhong et al in 2017 show that discs can heal on their own over time. In fact, “worse” herniations are more likely to heal.
- Size doesn’t always matter. Karppinen et al in 2001 reported that “the degree of disc displacement.. in MRI did not correlate with sciatic symptoms.”
- A well known systematic review in 2015 by Brinjikji et al demonstrated how common it is to have these changes on MRI and no symptoms whatsoever, even in our 20s, and especially as we age.
Can Your Disc Slip?
No. I don’t know the origin of this phrase, but it’s just referring to a disc herniation. I’m not a fan of it because I think it can create some misinformation and unhelpful visuals of what’s happening in your back. Your disc doesn’t slip and go anywhere. It’s still there doing it’s job.
Is Your Nerve Trapped or Pinched?
I think this is the most important of the three questions in this section. You might read or hear about your symptoms being caused by the nerve being trapped or pinched which seems like a very straightforward process, but it’s a bit of an oversimplification because nerves get compressed, pushed, pulled, bumped, etc. all day long, and most of the time you don’t notice.
Sometimes you might, though. For example, you sit on the toilet too long watching YouTube videos and your leg goes numb from the prolonged compression and lack of blood supply. Or you bump your “funny bone”, which is actually your ulnar nerve, and you get a nice zing! Neither one is problematic or causes long-term damage.
That paper by Karppinen and colleagues also showed that more compression of the nerve on MRI doesn’t necessarily mean worse symptoms. A 2006 paper by Rijn et al showed that patients who had symptoms in one leg might not have symptoms in the other leg despite showing compression of the nerve on the other side as well. Inflammation, swelling, and other factors play a role in this complex process.
Why is all of this important to know? Because the MRI might not exactly match what you’re experiencing. Therefore, unless you intend to get surgery, it’s not usually necessary to get an MRI because
- It doesn’t change management.
- It can create unnecessary fear.
- And it can create an unnecessary focus on the image. Benson et al in 2010 reported that “there was a poor correlation between clinical improvement and the extent of disc resolution,” so the goal of rehab shouldn’t be about changing what is shown on the MRI. The goal of rehab is to improve your function.
What Should You Expect From Your Doctor or Physio?
Based on an article by Stynes et al in 2018, your healthcare provider might ask you certain questions to identify if your symptoms are stemming from an irritated nerve in the low back.
- Do you have any pins and needles or numbness in your leg?
- Do you have pain below the knee?
- Is your leg pain worse than your back pain?
They’ll also do specific tests to assess the function of the nerve.
- They’ll check to see if your sensation is intact and normal.
- They’ll check the strength of your muscles.
- They’ll check your reflexes.
- They’ll likely do a straight leg raise or slump test to see if that movement increases your symptoms.
You might be wondering how these questions and tests relate to an irritated or sensitive nerve in the low back. Well, the nerves that originate in the low back actually travel all the way down the leg and if they’re not functioning at 100%, you might have more pain in the leg than the low back and have changes in sensation, strength, and reflexes.
They’ll probably ask you other questions as well and even if something seems really odd or irrelevant to you, I recommend sharing as much information as possible with your healthcare provider because that information might actually be very valuable to them.
Is There A Best Exercise?
No. There isn’t going to be one exercise or routine that works across the board for all people and all symptoms in all scenarios. You’ll come across resources on YouTube that promise a quick fix and I think it’s amazing when people do find relief with those videos, but it’s important to set realistic expectations because although sciatica has a generally favorable time course, symptoms don’t always quickly resolve and for some people, actually become persistent or episodic.
There are generally three camps of exercises:
- Trunk strengthening exercises, oftentimes in reference to Stuart McGill’s big 3 – bird dogs, curl ups, and side planks – which are performed daily as isometric holds within tolerance.
- Nerve glide variations that are prescribed with the intention of reducing the sensitivity of the nerve with different movements.
- Repeated motions, or you might have heard this be called the McKenzie method. A simplified explanation is that you repeat movements in the direction that improves your symptoms. Lumbar flexion is when you reach for your toes and your low back rounds. Lumbar extension is when you bend backward and your low back arches. In this example, you might try bending forward 10 times and then bending backward 10 times. If bending forward worsens your symptoms and bending backward improves your symptoms, then you would try to take advantage of that. Periodically throughout the day, in standing or on your stomach, you might repeatedly extend your back for a short duration of time depending on how you respond. If it helps and your tolerance to extension improves, then you might increase the amount of repetitions or the range of motion over time. You can do the same thing if your symptoms are worse with extension and better with flexion.
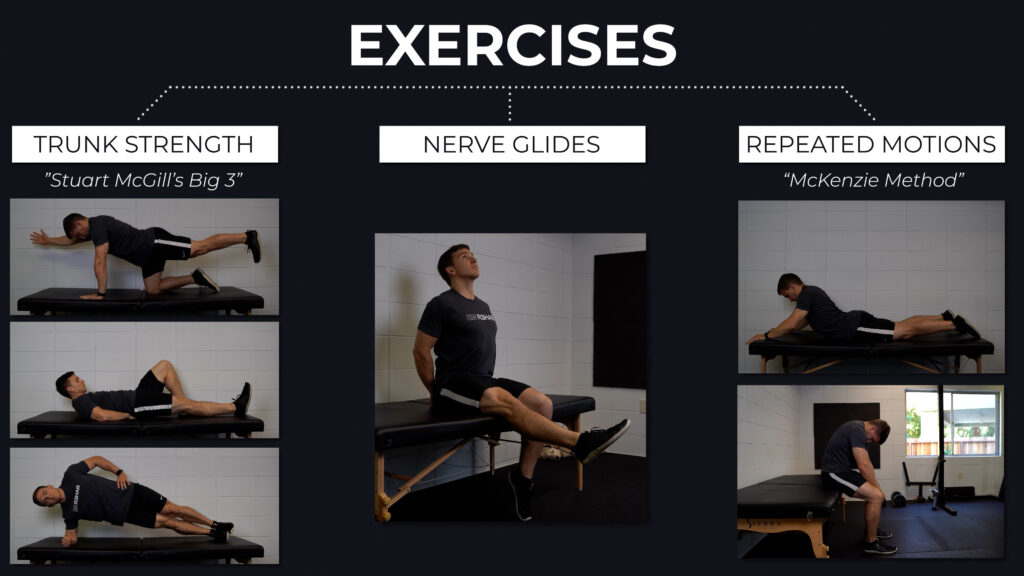
As I mentioned, no single approach is going to work for everyone. And for that reason, one of the approaches, or a combination of the three, might work for anyone. However, it’s not necessarily due to the mechanisms that they propose such as improving core stability, un-trapping the nerve, or pushing the disc material back in. Remember, the goal of rehab is to improve your function and how you feel. It doesn’t need to be much more complicated than that.
Based on a theoretical framework and some mechanistic research, I actually have a strong bias toward walking. I think it can be helpful to go for a walk first thing in the morning and periodically throughout the day. They can be short 5-10 minute walks to start, spaced out every few hours, and then you can slowly increase the time or distance. There’s virtually no harm and potentially a lot of benefit in building up to 3 20 minute walks per day. I highly recommend tracking your daily steps as an objective measure that you can slowly progress over time.
Are There Exercises That You Need To Avoid?
Maybe temporarily, but nothing has to be off limits permanently. Running, cycling, lifting weights, and other activities can actually be healthy for the discs and spine. The other goal of rehab is getting you back to doing what you love. You might have to scale back initially and make some modifications, but nothing has to be avoided forever. For example, if barbell back squatting at relatively higher loads and lower reps is problematic, you might try upright split squats at relatively lower loads and higher reps. Or if conventional deadlifting from the floor is an issue, you can deadlift from blocks, switch to a trap bar, or perform accessories that train similar muscle groups.
Is Sciatica Preventable or Avoidable?
Systematic reviews by Cook et al in 2014 and Parreira et al in 2018 give us some insight into the modifiable risk factors associated with sciatica such as smoking and obesity. Many of the recommendations here are the same across a spectrum of injuries or conditions – don’t smoke, eat well, exercise regularly, stress less, sleep enough, and do things in moderation. Easy for me to suggest, but obviously hard to implement. However, the videos that tell you to do this one exercise every day for the rest of your life probably aren’t very helpful.
Is Surgery A Good Option for Sciatica?
A paper by Peul et al in 2007 and a systematic review by Fernandez et al in 2016 suggest that surgery might provide better short-term relief and faster recovery, but on average, long-term outcomes between surgery and non-surgical management are similar. Therefore, non-surgical management is going to be preferred in most cases because surgery doesn’t guarantee success, it comes with its own risks and costs, and outcomes are similar after one year. However, I am a physical therapist and not an orthopaedic surgeon, so please discuss options with your medical doctor.
Sciatica Summary
Sciatica is a word often used to describe symptoms in the leg such as pain, weakness, and numbness which may involve an irritated nerve in the low back secondary to a disc herniation. The good thing though is that your discs don’t slip, they’re not fragile like jelly doughnuts, and symptoms can completely resolve on their own without the need for surgery or special treatments. An exercise program can supplement your goals and recovery, but there isn’t always a quick fix or a BEST exercise so it’s important to set realistic expectations that this process can take some time. As with any injury, I recommend seeking out a healthcare provider such as a physical therapist.
Don’t forget to check out our Low Back Resilience Program!
Disc Herniations, Multifidus, Lumbar Stenosis
Thanks for reading. Check out the video and please leave any questions or comments below.